Scientific Journal of Genetics and Gene Therapy
Triplet with Dicephalus Twins: A Case Report
Adeku MA1,3, Ajayi GO1,2*, Adegbola O1 and Adeyemi A2
2Prenatal Diagnosis and Therapy Centre, College of Medicine, University of Lagos, PMB 12003, Surulere, Idi-Araba, Lagos, Nigeria
3State Hospital, Otta, Ogun State, College of Medicine, University of Lagos, PMB 12003, Surulere, Idi-Araba, Lagos, Nigeria
Cite this as
Adeku MA, Ajayi GO, Adegbola O, Adeyemi A (2017) Triplet with Dicephalus Twins: A Case Report. Scientific J Genet Gene Ther 3(1): 001-003. DOI: 10.17352/sjggt.000012Nigeria is known to have the highest twining rate in the world. In this report, we present a case of a woman MS, 32 years old, Gravida4, Para3 (3alive), who had caesarian section for conjoined twin (thoracopagus) and malformed triplet on 26/3/2015 at 21 weeks of gestation. There was no history of usage of teratogenic drugs and all previous deliveries were spontaneous vaginally. The ultrasound done on 24th March 2015 showed a viable conjoined twins, with thoraces fused together but with separate active heart actions. The limbs appeared to be just a pair, like in normal singleton and a non-viable mummified triplet. Placenta was anterior, polyhydramnios BPD 55mm composite to gestational age as of 21 week and 6days and Estimated date of delivery (EDD) of 22/07/15. The live babies conjoined twins died 3 minutes post-delivery caesarian section. The post-operative phase was without complications and the mother was discharged home on the 30/03/15 and did not show up for post natal care.
Introduction
Conjoined twins or Siamese twins are identical twins whose bodies are joined to varying extent in utero. It is a rare phenomenon which occurs in approximately 1:40, 000 births, but only 1:100,000 to 1:200, 000 live births. It is commoner in female births, with a female to male ratio of 3:1 [1,2].
Conjoined twins are monozygotic, mono-amniotic and monochromic and always of the same gender. Two different theories have been proposed to explain the origin of conjoined twins. The first older and most commonly accepted theory is that of fission, in which the fertilized ovum split partially. The second later theory is that of fusion, in which the fertilized egg completely separate, but stem cell find like stem cells on the other twin and fuses the twins together.
40- 60% conjoined twins are stillbirth, 35% of twins that survive die within the first 24 hours due to abnormalities incompatible with life. The overall survival rate is put at 25% - [1,3,4]. It is believed to be common in Southern Asia and Africa [1]. The birth rate of conjoined twins in Africa in 1.14,000 births, and 1:400 identical twin pregnancies is conjoined twins. The incidence of normal twining rate in Nigeria is the highest in the world. The highest reported rate in Nigeria [is 1:20-22 from the South West [5,6].
The incidence rate in conjoined twin in Nigeria is not known for now, though a number of cases have been reported [7-12].
There are many types of conjoined twins based on the point at which they joined. More than 36 separate types had been identified. The common ones are Thoraco-omphalopagus (28%), Thoracopagus (18.5%), Omphalopagus (10%), Parasitic twin (10%), Craniopagus (6%). Leacham proposed a system of classification in attempt to standardize classification of conjoined twins [1-3]. Dicephalus twins have single trunk and two heads. They are classified into five subtypes:
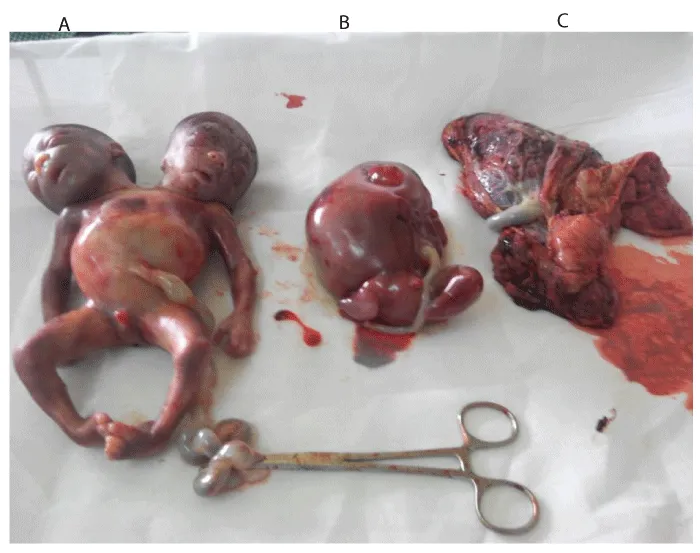
A case of conjoined twins with trunks, two heads, two feet, two arms and tribrachus with a non-viable mummified triplet is being reported from Prenatal Diagnosis and Therapy Centre of a Tertiary Hospital in Lagos.
Case Report
Siamese twins, which are now synonymous for conjoined twins were delivered in Siam, now Thailand were named Chang and Eng Bunker (1811-1874) is the most famous of all conjoined twins reported on.
MS, 32 years old now P4+1, a woman who has caesarian section for conjoined twin (thoracopagus) and malformed triplet on 26/3/15 at ultrasound gestational age of 21weeks. She registered for antenatal care on 19/03/15 one week prior to delivery at gestational age of about 20 weeks with LMP(Last Menstrual Period) 2/11/14 with a booking Packed Cell volume of 38%, blood group A+ve, genotype AA, RVD(Retro-viral diseases) negative, booking BP 110/60mmHg and normal urinalysis. Pregnancy was spontaneously conceived. She is not known as hypertensive or diabetic, no history of teratogenic drugs usage or herbs used and no history of viral infection in index pregnancy. All previous deliveries were SVD (Spontaneous Vaginal Delivery) all alive and well.
She was subsequently asked to do an urgent obstetric scan. This was done on 23/03/15 and showed a viable conjoined twin with hyper extended head and neck. The thoraces were fused together but with separate active hearts. The limbs appeared to be just a pair, like a normal singleton gestation.
Also noticed is a non-viable mummified triplet. Placenta was anterior, normal in thickness with grade 1 maturity. There was polyhydramnios and biometry is as follows: BPD-55mm, Femur Length (FL) 34mm giving composite gestational age of 21+6 weeks and EDD of 22/7/15.
Conclusion of case report: Gross fetal anomaly (conjoined twin) with demise of a triplet. A second opinion scan was sought same day and revealed similar findings.
She subsequently has caesarian section and evacuation of product of conception on 26/3/15/. Under general anesthesia (GA), intra-operative findings were as follows:
• Clean pelvis with poorly formed lower uterine segment
• Anterior placenta, ragged, polyhydramnios
• Live conjoined twin with two separate heads and a single chest wall, abdomen, a male genitalis and two upper and lower limbs with active cardiac activity until few minutes after birth.
• A third abnormally formed triplet with no distinct head, rudimentary thorax, and abdomen with no limb, eye and ear buds.
• Estimated Blood Loss (EBL) was 400mls with a satisfactory post-operative state.
The live babies (conjoined twin) died about 3 minutes after birth and were immediately transferred to the mortuary.
The mother fared well post-operatively and was discharged home on 30/3/15 which was the 4th day post-operative with Blood Pressure 110/70mmHg and Packed Cell Volume of 36%. She never showed up for the postnatal visit i.e. lost to follow up.
We reported a case of triplet with dicephalus twin delivered by caesarean section alive but died three minutes after birth. This is quite different from others reported from Nigeria that was diagnosed at delivery [8,9,13]. The diagnosis was made prior to delivery through ultrasound findings, which emphasize the role of routine ultrasound in an obstetric care. High resolution ultrasonography can detect conjoined twins as early as the eight weeks of gestation. The clinical sign indicative of conjoining of twins on ultrasound are: inability to separation fetal bodies, lack of separating membrane, three or more umbilical cord vessels, or alternatively 2 vessels umbilical cord, both fetal heads in same plane, usual backward flexion of the cervical spine, no change in the relative maternal movement and maternal manipulation and inability to separate fetal bodies after careful observation. The fetus can then be evaluated to assess the possibility of postnatal survival using echocardiography and ultrafast magnetic resonance imaging [14-16].
Delivery route depends on the gestational age at presentation. Before 24 weeks gestation, vaginal delivery is been recommended while caesarean section is recommended in the third trimester deliveries because of the high incidence of obstructed labor and resultant fetal damage as well as risk of maternal morbidity [9,10,13]. For now, only one case of spontaneous natural delivery of live conjoined twins has been reported in Nigeria [17].
Destructive surgery with the aim of vaginal delivery was not contemplated because of maternal injury. Survival is closely tied to the extent of organ sharing between conjoined twins. Separation of conjoined twins may involve relatively simple to extremely complex surgery, depending on the point of attachment and extent of organ sharing and involves multidisciplinary team approach [4,18,19]. Surgical separation can be extremely risky and life – threatening, occasionally resulting in the death of one or both of the twins. Most cases of dicephalus dipus tribrachus are stillborn or die shortly after birth and pathological examination reveals extensive vital organ sharing and congenital malformations. Hence, separation is usually not completed in them.
Associated anomalies with conjoined twining are duplication of visceral organs omphalocele, facial cleft, meningomylocele, skeletal anomalies, imperforate anus and cardiac defects [20]. In our case, pathological anatomy could not be done to ascertain associated anomalies as parents decline pathological and radiological examination.
In conclusion, antenatal care for all pregnant women cannot be over-emphasized. Antenatal ultrasound examination should be routinely done as part of screening for congenital abnormalities and early referral to appropriate level of care.
- Conjoined twins. Link: https://goo.gl/w4wgVd
- Yuliya Burmagina (2006) Duplicata incompleta, dicephalus dipus dibrachius. Link: https://goo.gl/eTbWR2
- James LS, James TG (2006) The Crainopagus malformation: Classification and implications for surgical separation. Brain 129: 1084-1095. Link: https://goo.gl/EceBAv
- Adejuiyigbe O, Sowande OA, Olabanji JK, EO Komolafe, F Faponle, et al. (2005) Successful separation of two pairs of conjoined twins in Ife: Nigeria case Report. East Afri med J 82: 50-54. Link: https://goo.gl/1f4hPJ
- Abudu OO, Agarin M (1983) Twin Pregnancy and Perinatal mortality in Lagos. J Obstet Gynae East Afri 3: 7-11.
- Abudu OO (2006) Multiple Pregnancy In: Textbook of Obsteristic and Gynecology for Medical Students. 2nd Edition, Editor: Akin Agboola Publication 373-380 Heinemann Educational Books (Nigeria) Plc. 2006: 373 – 380.
- Mabogunje OR, Lawrie JH (1980) Conjoined twins in West Africa. Arch Dis Child55: 626-630. Link: https://goo.gl/nczHgN
- Aiyedun TA (2002) The conjoined twins of Gusau, Nigeria. WAJM 21: 256-257. Link: https://goo.gl/J4TPoa
- Owolabi TA, Oseni SBA, Sowande OA, Adejuyigbeo, Edward O Komolaf, et al. (2005) Dicephalus Dibrachius Dipus Conjoined Twins in a Triplet Pregnancy. Trop J Obstet Gynaecol 22: 87-88. Link: https://goo.gl/rdy1Yx
- Ibekwe PC, Onuoha CEO (2008) Spontaneous vaginal delivery of undiagnosed Bipagus conjoint twins. Annals of African Medicine 7: 50-51. Link: https://goo.gl/bxjwPh
- Omokhodion SI, Ladipo JK, Odebode TO, Ajao OG, Famewo CE, et al. (2001) The Ibadan conjoin Twins: A report of Omphalopagus Twins and a review of cases reported in Nigeria over 60 years. Annals of Tropical Paediatrics 21: 263-270. Link: https://goo.gl/Cr6Dey
- Adetoye D, Aigoro NO, Onabadejo AA, Erinoso A (2011) Dicephalus Twins- A case Report. Nigerian Medical Practitioner 59: 51-53. Link: https://goo.gl/6B3fRb
- Adetoye D, Aigoro NO, Onabadejo AA, Erinoso A (2011) Dicephalus Twins- A case Report Nigerian Medical Practitioner 59: 51-53. Link: https://goo.gl/6B3fRb
- Goldberg Y, Ben-Shlomo I, Weiner E, Shaley (2000) First trimester diagnosis of conjoined twins in a triplet pregnancy after IVF and ICSI. Human Reproduction. Case Report 15: 1413-1415. Link: https://goo.gl/fgmZDB
- Shah DS, Tomah G, Preetrikiran, Prajapati H (2006) Conjoined Twins: Report of two cases. Ind J Radio Imag 16: 199-201. Link: https://goo.gl/DrX4kV
- Ratner AN, Terrone D, Cosgrove J (2006) Thoracopagus coined twins. JDMS 22: 2253-2255. Link: https://goo.gl/SgJKxr
- Ibekwe PC, Onuoha CEO (2008) Spontaneous vaginal delivery of undiagnosed bipagus conjoint twins. Annals of African Medicine 7: 50-51. Link: https://goo.gl/vdH4LZ
- Rode H, Fieggen AG, Brown RA, Cywes S, Davies MRQ, et al. (2006) Four decades of conjoined twins at the Red Cross children Hospital Lessons learned. SAMI 96: 931-940. Link: https://goo.gl/7N55fG
- Shijia JK, Ngiloi PJ (2000) Final Stage Surgical Treatment of the conjoined twins of Masasi; Tanzania: A case Report. East Afri Med J 17: 172-173. Link: https://goo.gl/jPV1mH
- Sangari SK, Khatri K, Pradhan S (2000) Omphalopagus Ischiopagus Tetrapus Conjoined Twins- A case report. J.Anat.Soc.India 50: 40-42. Link: https://goo.gl/R44aDK
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
