International Journal of Radiology and Radiation Oncology
Primary paraspinal hydatid cyst with intraspinal extension. A rare case report
Saman Anwar*, Ayesha Shayan, Hina Naseer, Azzan Mujahid, Rabia Ahmed and Bushra Shamim
Cite this as
Anwar S, Shayan A, Naseer H, Mujahid A, Ahmed R, et al. (2023) Primary paraspinal hydatid cyst with intraspinal extension. A rare case report. Int J Radiol Radiat Oncol 9(1): 013-017. DOI: 10.17352/ijrro.000052Copyright License
© 2023 Anwar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Hydatid cyst is a zoonotic disease caused by Echinococcus granulosus. It rarely presents in the musculoskeletal system. Primary hydatid disease in paraspinal muscles is very rare. It can be discovered as an incidental finding in radiological imaging. Symptomatic patients are presented with usually symptoms secondary to the compression effect. It can cause dreadful consequences like erosion of adjacent bones, myelopathy, and cauda equine syndrome if left untreated. We present such a case of Primary Paraspinal Cyst with Intraspinal Extension, and its radiological imaging findings, including X-ray, CT scan, and MRI.
Introduction
Hydatid disease is caused by infection with Echinococcus granulosus, the larval stage of long tapeworm [1-3]. Liver, lung, and spleen are the common sites of primary hydatidosis. Occasionally parasites infect other organs by entering the systemic circulation and disseminating throughout the body. Musculoskeletal involvement is usually secondary and not common with an incidence of less than 2.5% and may affect the pelvis and sacrum, metaphyses of the long bones, skull, spine, and ribs [3,4]. Primary hydatidosis is extremely rare in the musculoskeletal system, especially muscles, with only a few cases reporting primary paravertebral muscle involvement [4,5]. In literature, only less than 0.5% prevalence is reported in paraspinal muscles [6]. Primary involvement being rare in skeletal muscles, may cause diagnostic problems [7]. Patient may present with chronic lower back pain or swelling in the thoracolumbar area. The intraspinal extension may result in myelopathy or cauda equina syndrome [8]. Diagnosis can be established by clinical findings and various radiological modalities like ultrasound, CT scan, and MRI. While MRI is considered the technique of choice. Usually confirmed by histopathological correlation. Surgical excision combined with medical treatment remains the definitive treatment option [6-8].
Literature review shows such cases that presented clinically with lower back pain or various neurological symptoms and imaging showed a multiseptated paraspinal mass which may or may not show spinal compression or intraspinal extension. These, later on, underwent surgery and were proved as hydatid cysts on histopathology [4,5,9,10].
Here we present a rare case of primary hydatid disease in paraspinal muscles with intraspinal extension that we came across in our hospital.
Case report
65 years old male presented in the outpatient department of neurosurgery with a complaint of backache in the dorsolumbar region radiating to the right leg for 4 months and paraplegia for the past 20 days. He had complained of on-and-off low-grade fever for the past 20 days Initially the pain was in the lower back that failed to resolve despite taking medication. Gradually it started radiating to both legs and became severe enough to disturb the normal routine finally resulting in paraplegia and urinary retention.
On examination, he was conscious and well-oriented. There was decreased power, 0/5 in the right and 1/5 in the left lower limb. Reflexes were also decreased in bilateral lower limbs. His upper limbs had a power of 5/5 and his reflexes were intact. His sensations were also intact. The patient had lost sphincter control. Saddle anesthesia was present. The rest of the examination was unremarkable. No swelling was noted.
Initially, as a part of his primary workup, an X-ray (Figures 1a,1b) of lumbosacral spine anteroposterior and lateral views were done which showed a large faint soft tissue density mass with internal multiple rounded cystic areas and patchy calcifications on right side of the abdomen (Figure 1a). It was displacing the large bowel loops towards the left side. This was associated with scoliosis of the lumbar spine with its convexity towards the left side. There was scalloping, irregularity, and erosion of L1 and L2 vertebral bodies along their right lateral aspect. There was reduced vertical height of the L2 vertebral body with erosions along its superior and inferior endplates as well (Figure 1b). This gave the impression of a paraspinal hydatid cyst.
And further evaluation with MRI was advised to look for the extent of the disease. X-ray Chest, Ultrasound whole abdomen, and a CT scan of the patient were also done for further evaluation and to rule out the presence of disease elsewhere.
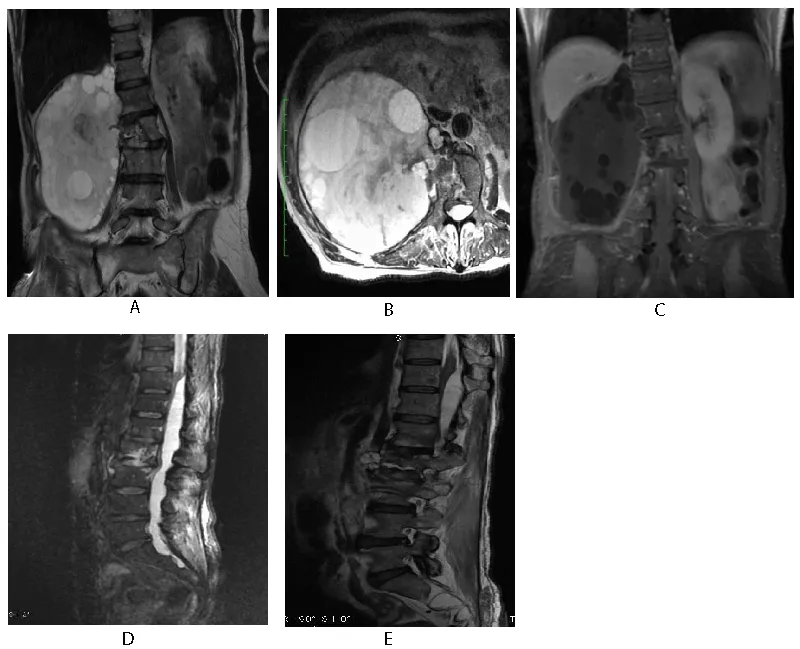
MRI lumbosacral spine with and without contrast enhancement (Figures 2a-2e) was done which showed gentle scoliosis of the dorsolumbar spine with its curvature towards the left. A large well-defined multivesicular cystic area was seen in the right paraspinal region (Figure 2a) involving the proximal part of the psoas muscle. It was extending from levels of D11, and D12 to S1 vertebrae with no post-contrast enhancement (Figure 2c). This represents a hydatid cyst with multiple daughter cysts. It was causing anterior displacement of the right kidney (Figure 2b). It was also causing scalloping of the right lateral border of the L1 vertebral body and significant erosion of the right half of the L2 vertebral body involving its inferior end plate (Figure 1a).
An intraspinal extradural cystic area was seen extending from the level of the D11 to the S2 vertebra. It was causing significant compression and anterior displacement of the thecal sac, distal spinal cord, and cauda equina (Figures 2d,2e). It measured about 1.6 x 2.2 x 20.0 cm (anteroposterior x transverse x craniocaudal). This represents the intraspinal component of the hydatid cyst. High signals were seen in the spinal cord at the level of D10 representing cord edema. The cyst showed mild protrusion into the right neural foramen at the level of D12/L1 and mild extension through the left neural foramen at the level of L2 and L3 vertebrae. Few septations were seen in its caudal end at the S1 level.
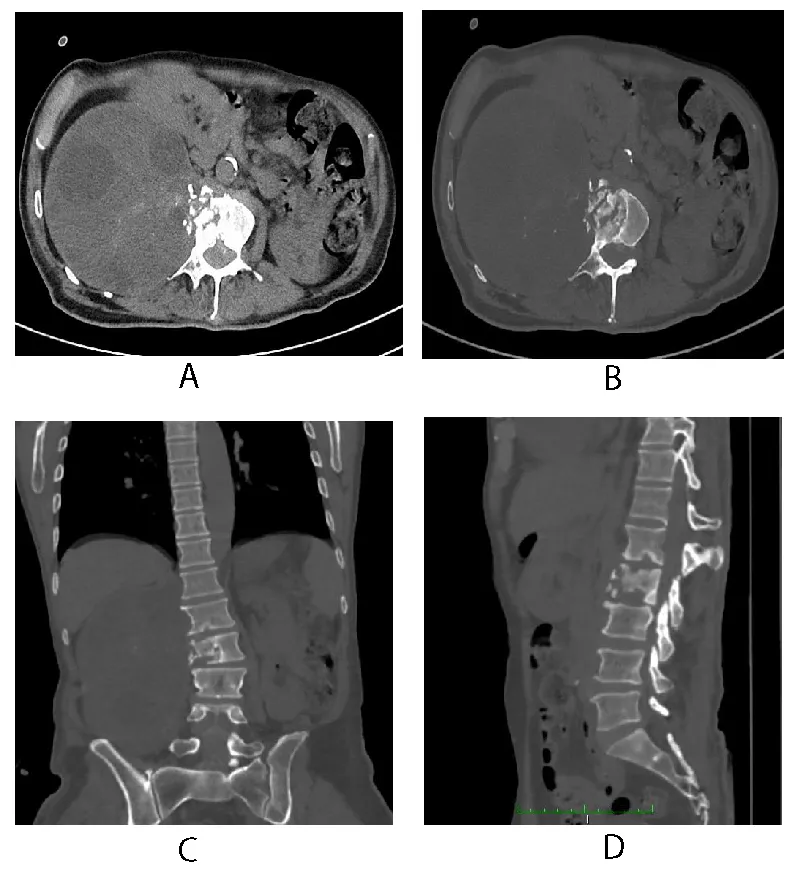
CT scan of the lumbosacral spine (Figures 3a-3d) was also done to see the extent of vertebral involvement. A large well-defined cystic area containing multiple small cysts was also seen in the CT scan likely representing a hydatid cyst (Figure 3a). It contained patchy foci of internal and peripheral calcification. The proximal part of the right psoas muscle was seen as involved. Medially it was causing erosion and destruction of the L2 vertebral body with extension into the spinal canal at this level (Figures 3b,3c). It was also causing scalloping of the lateral border of the L1 vertebra. It was displacing the right kidney anteriorly. It was also abutting the anterolateral abdominal wall resulting in a significant bulge with intact fat planes (Figure 3a). Cyst was also abutting the posterior abdominal wall and causing scalloping of the inferior margin of the liver with intact fat planes (Figure 3c). It was displacing the hepatic flexure in ascending colon inferiorly.
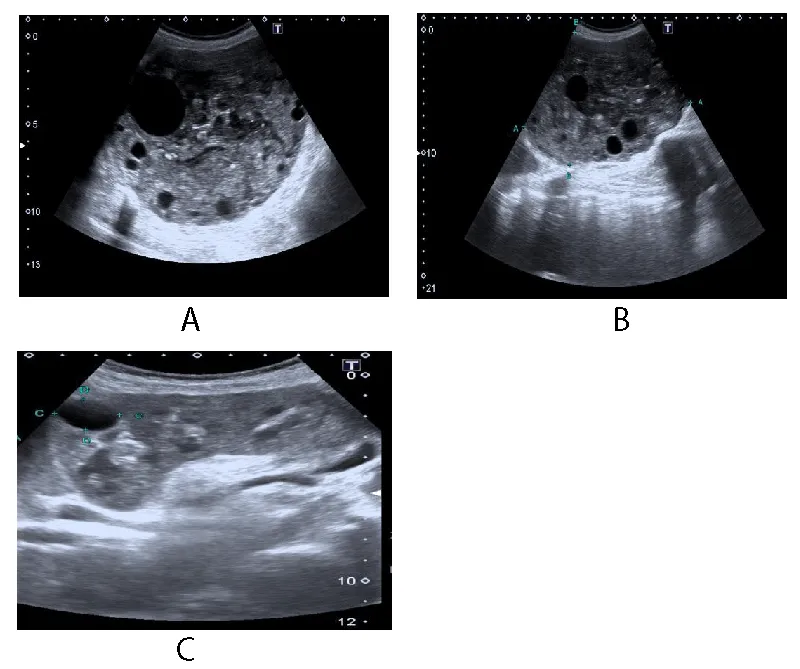
Concomitantly performed ultrasound (Figures 4a-4c) also demonstrated the hydatid cyst in the right hypochondrium extending into the right lumbar region. It was causing compression of the inferior margin of the liver and displacing the right kidney anteriorly.
X-ray chest (Figure 5) of the patient was also done which showed no signs of Hydatidosis.
Based on these radiological imaging, a diagnosis of primary paraspinal hydatid cyst with intraspinal extension was made.
His baseline laboratory investigations were within the normal range and were non-contributory to our diagnosis. However, Echinococcus antibodies were detected in serum which further strengthened our diagnosis.
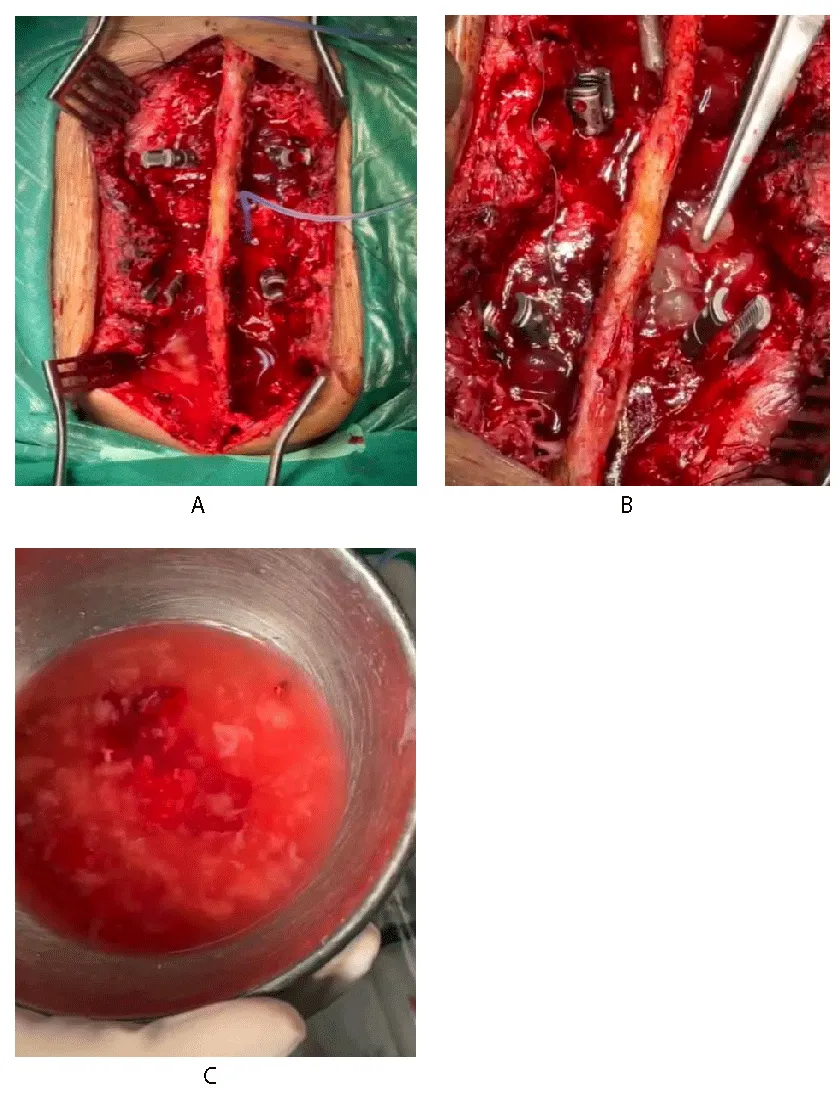
The patient was admitted under the care of the neurosurgery team and surgical excision of the hydatid cyst was planned. After written and informed consent, baseline investigations, pre-operative workup, and general anesthesia fitness he was booked for elective surgery and shifted to Operation Theater. He underwent D11, D12, and S1 laminectomy followed by complete excision of both paraspinal and intraspinal components of the cyst. Multiple daughter cysts were delined from the extradural compartment (Figures 6a-6c). L1/L3 pedicle screw fixation was done.
Histopathological examination confirmed the presence of hydatid disease.
The patient went through a smooth recovery with no drastic or minor complications on antibiotics and symptomatic treatment in the hospital post-operative course and on follow-up visits. Post-operative radiological imaging showed no evidence of recurrent or residual lesions.
Discussion
Hydatid disease or Echinococcosis is a disease caused by the larval form of a long tapeworm Echinococcus granulosus. Its life cycle involves a definitive host like a dog, wolf, or other carnivore. It lives parasitically in the intestine of its definitive host. The infection is usually transmitted to humans through infected animals via their feces and eggs [2,3].
A Hydatid cyst is formed of a fluid-filled cavity that is lined by three layers, the outermost, pericyst (host reaction), the middle layer, ectocyst (laminated membrane), and the inner layer, endocyst (germinal layer). The endocyst gives rise to laminated membranes and secretes hydatid fluid [7].
The disease is distributed worldwide, however, it is endemic to the temperate climate [3,4]. It can occur in any age group affecting people in their third and fourth decades of life commonly having almost equal gender distribution with slight female predilection [11].
Hydatid disease can involve almost every part of the body except a few [6,7], the liver (59% - 75%) and lungs (27%) being the most commonly involved organs. The other organs of involvement are the kidney (3%), bone (1% - 4%), brain (1% - 2%), heart, spleen, pancreas, breast, and muscles [7]. Musculoskeletal involvement is seen rarely and accounts for 0.5% - 5% of cases of hydatid cysts and is almost always secondary to infection of other organs like the liver or lung. Primary musculoskeletal involvement is rare [4]. Primary paravertebral muscle hydatid cyst extending to neural foramina without the presence of disease elsewhere in the body is a very rare condition even in endemic areas [5].
Hydatid cysts are slow-growing cysts [7,11] that may remain asymptomatic for many years and are usually detected incidentally. Or these may be detected usually secondary to the compression symptoms as cysts grow in size. The symptoms also depend on the organ of involvement like sputum, dyspnea, hemoptysis and chest pain in pulmonary hydatid [11], right upper quadrant pain, jaundice or palpable mass in hepatic involvement, left upper quadrant pain in splenic involvement, swelling, and pathologic fracture in musculoskeletal involvement, headache, and pressure symptoms in intracranial involvement [11,12] and persistent lower backache and neurologic deficits in case of spinal involvement.
Various serological investigations and imaging tools are used to establish the diagnosis. The serological tests detect specific circulating antigens or serum antibodies that include ELISA for Echinococcal IgG (sensitivity 95%, specificity 94%),16 Immunoelectrophoresis (IEP), Haemagglutination tests, etc. Various imaging modalities like Plain X-ray, Ultrasonography, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI) can help us to establish the diagnosis with high accuracy by direct visualization of the cyst, identifying its characteristic features [7,11].
It may demonstrate various characteristic imaging features depending on the site of involvement, stage of growth, complications, or hematogenous spread. Radiography, Ultrasonography (USG), Computed Tomography (CT), and Magnetic Resonance Imaging (MRI) are frequently used imaging modalities. Radiography is mostly helpful in pulmonary disease and for demonstrating calcification in the cyst. The characteristic ultrasonographic findings are cystic nature, daughter vesicles, membranes, septa, and hydatid sand. Modalities of choice remain CT and MRI as these are more helpful in identifying number, size, anatomic location, identification of local complications, and systemic spread. CT scan is of particular help in case of bony involvement. MRI is helpful in cases of biliary and neurological involvement [13].
In cases of spinal involvement, plain radiographs may show well-defined, multiple, expansile, osteolytic cavitary lesions with no sclerosis or periosteal reaction. Plain radiographs may show the involvement of adjacent vertebral bodies and their posterior elements. Ultrasonography of the abdomen usually may not reveal any other abdominal organ involvement. A CT scan may show multiple cystic, osteolytic expansile lesions in vertebral bodies with no enhancement on postcontrast images. MRI may show multiple cystic fluid-filled lesions with thin walls at multiple levels in the spine. Intraspinal extension may also be seen in some cases. Paravertebral muscles may show multiple spherical large cystic lesions with daughter cysts inside [3]. As in our case, many of these characteristic findings were present. The lower incidence [6,10,14] and classical presentation in our case make it more interesting.
Treatment options depend on the site, size, and clinical presentation of the patient [15]. Albendazole can be used to treat the patient medically but in most cases, surgery remains the mainstay of treatment as we did in our case [6,11,15].
Conclusion
Hydatidosis is a zoonotic disease caused by larva of Echinococcus granulosus that may present in any age group but usually presents in the third to fourth decade of life with a slight female predilection. It is a slow-growing disease that can involve almost every organ of the body except a few. The clinical presentation usually depends on the site of involvement, however, it may remain asymptomatic for many years. Many laboratory tests and imaging modalities are used to reach a definitive diagnosis. Although may be treated medically but requires surgical intervention in most of the cases for definitive treatment.
Ethical review
This case report was written and radiological images and surgical and histopathological findings were added after taking consent from the patient. The patient’s identity is not shown here and will be kept confidential.
- Prevention C. C for DC, 2023. CDC—Echinococcosis. https://www.cdc.gov/parasites/echinococcosis/index.html
- PUMP KK. Echinococcosis (hydatid disease): a review and report of a case of secondary echinococcosis. Can Med Assoc J. 1963 Jul 13;89(2):73-8. PMID: 13972527; PMCID: PMC1921605.
- Prabhakar MM, Acharya AJ, Modi DR, Jadav B. Spinal hydatid disease: a case series. J Spinal Cord Med. 2005;28(5):426-31. doi: 10.1080/10790268.2005.11753843. PMID: 16869090; PMCID: PMC1808269.
- Sadeghian H, Motiei-Langroudi R. Hydatid Cyst in the Lumbar Paravertebral Muscle: A Case Report. Cureus. 2019 Aug 9;11(8):e5353. doi: 10.7759/cureus.5353. PMID: 31608188; PMCID: PMC6783210.
- Bulut HT, Yildirim A, Celik T, Baykan AH, Sürücü GD, Ekmekçi B. Hydatid cyst of paravertebral muscle mimicking disc herniation. Spine (Phila Pa 1976). 2013 Aug 15;38(18):E1175-7. doi: 10.1097/BRS.0b013e31829a8357. PMID: 23680835.
- Khorshidi H, Taghipour M, Moslemi M, Farsangi LE. Hydatid cyst of para-spinal muscles as a rare cause of back pain in a woman: a case report and review of literature. Case Reports in Clinical Medicine. 2020 Jun 29 [cited 2023 Jan 19];9(7):184–90. http://www.scirp.org/Journal/Paperabs.aspx?paperid=101370
- Parray FQ, Ahmad SZ, Sherwani AY, Chowdri NA, Wani KA. Primary paraspinal hydatid cyst: a rare presentation of Echinococcosis. Int J Surg. 2010;8(5):404-6. doi: 10.1016/j.ijsu.2010.04.011. Epub 2010 May 26. PMID: 20561990.
- Zairi M, Boussetta R, Msakni A, Sahraoui G, Mohseni AA, Nessib MN. Infected primary hydatid cyst of the right lumbar paraspinal muscles: A rare case in a ten-year-old child. Int J Surg Case Rep. 2021 Dec;89:106570. doi: 10.1016/j.ijscr.2021.106570. Epub 2021 Nov 3. PMID: 34837856; PMCID: PMC8632840.
- Singh N, Anand T, Singh DK. Imaging diagnosis and management of primary spinal hydatid disease: a case series. Egyptian Journal of Radiology and Nuclear Medicine. 2022 May 10 [cited 2023 Jun 2];53(1):106. https://doi.org/10.1186/s43055-022-00785-1
- Karakasli A, Yilmaz M, Mucuoglu AO, Yurt A. A large primary dumbbell hydatid cyst causing neural foraminal widening of the thoracic spine: A case report and literature review. Int J Surg Case Rep. 2015;8C:55-8. doi: 10.1016/j.ijscr.2014.12.036. Epub 2015 Jan 16. PMID: 25625491; PMCID: PMC4353951.
- Baruah A, Sarma K, Barman B, Phukan P, Nath C, Boruah P, Rajkhowa P, Baruah M, Dutta A, Naku N. Clinical and Laboratory Presentation of Hydatid Disease: A Study From Northeast India. Cureus. 2020 Sep 5;12(9):e10260. doi: 10.7759/cureus.10260. PMID: 33042698; PMCID: PMC7537570.
- Geramizadeh B. Unusual locations of the hydatid cyst: a review from Iran. Iran J Med Sci. 2013 Mar [cited 2023 Apr 16];38(1):2–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3642939/
- Mehta P, Prakash M, Khandelwal N. Radiological manifestations of hydatid disease and its complications. Trop Parasitol. 2016 Jul-Dec;6(2):103-112. doi: 10.4103/2229-5070.190812. PMID: 27722098; PMCID: PMC5048696.
- Tian Y, Jiang M, Shi X, Hao Y, Jiang L. Case Report: Huge Dumbbell-Shaped Primary Hydatid Cyst Across the Intervertebral Foramen. Front Neurol. 2020 Nov 24;11:592316. doi: 10.3389/fneur.2020.592316. PMID: 33329343; PMCID: PMC7732459.
- Din DPMU, Anjum WA, Ahmad ML, Rehman KA, Ahmad GB, Gulshan WN. Primary para-vertebral hydatid cyst in the sub-occipital area of the neck: an unusual case of echinococcosis. Egyptian Journal of Neurosurgery. 2018 Sep 7 [cited 2023 Jun 2];33(1):16. https://doi.org/10.1186/s41984-018-0015-6
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
