International Journal of Radiology and Radiation Oncology
The Prognostic Value of Post-Void Residual Urine Volume, Abdominal Prostate and Transrectal Prostate Ultrasound for Complication of Benign Prostate Hyperplasia: A Case Report Sonographic Analysis
Ifeanyi Nicholas Malu*
Cite this as
Malu IN (2019) The Prognostic Value of Post-Void Residual Urine Volume, Abdominal Prostate and Transrectal Prostate Ultrasound for Complication of Benign Prostate Hyperplasia: A Case Report Sonographic Analysis. Int J Radiol Radiat Oncol 5(1): 001-007. DOI: 10.17352/ijrro.000032This case report aimed to evaluate the sonographic usefulness of gray-scale transrectal ultrasound (TRUS), transabdominal prostate ultrasound (TAPUS) and post-void residual (PVR) urine volume in the detection of an enlarged prostate. Benign prostate hypertrophy(BPH) is a common complaint in older men with clinical outcomes such as urinary hesitancy, bladder distention, and other signs of bladder outlet obstruction. The case presented describes a patient with urinary symptoms associated with an enlarged prostate and bladder obstruction. The results show that an enlarged prostate and bladder disease may be evaluated using post-void residual urine measurement of the bladder, abdominal prostate ultrasound and evaluation of the prostate using the transrectal ultrasound method. This case report will make an essential contribution to the existing literature and can enhance positive social changes by providing an in-depth understanding of the diagnostic capabilities of ultrasound technology in the evaluation of BPH.
Introduction
Benign Prostate Hyperplasia (BPH) is a frequently diagnosed condition for which ultrasound technology(UST) has a unique role in diagnosis. UST has been used in the area of prostate volume measurement, echotexture, and illustration of tissue stiffness or elasticity of the prostate gland. Although inexpensive and noninvasive, ultrasound technology is not associated with harmful radiation. After the urologist’s finger, ultrasound is the first line of diagnostic imaging used to detect an enlarged prostate.
BPH is a condition of older men, and its incidence has increased over the years. An enlarged prostate, also known as benign prostatic hyperplasia or benign prostatic hypertrophy is common as a man ages and is present in 50% of 60 years old increasing to 90% by age 80 years (Urology Care Foundation). Many researchers have noted the correlation between age and the prostate gland volume [1]. BPH is also the abnormal proliferation of prostatic cells associated with voiding dysfunctions such as lower urinary tracts infection including urinary retention. Although BPH is associated with quality of life issues, it is not life-threatening, and it does not lead to prostate carcinoma.
The prostate gland is part of the male urinary system. The primary function of the prostate is to make fluid for semen (National Cancer Institute, 2012). The prostate gland is located below the bladder, inferior to the seminal vesicles, anterior to the rectum and surrounds the urethra. The urethra is a thin-walled tube extending from the trigone to the external urethral orifice (National Cancer Institute, 2012). The tube passes vertically through the prostate gland. The prostate gland surrounds the bladder neck and urethra in men. Because of its position around the urethra, enlargement of the prostate quickly interferes with the regular passage of urine from the bladder. Its size changes with age but in adults, it is often about the size of a walnut (National Cancer Institute, 2012). At birth, the prostate is about the size of an almond.
BPH is diagnosed with the digital rectal examination(DRE), cystoscopy, transrectal prostate ultrasound and urodynamic, prostate-specific antigen(PSA), urinalysis and culture and bladder ultrasound. The symptoms vary, but most commonly involve changes or problems with urination. BPH is associated with incomplete bladder emptying, weak stream, hesitancy, urinary frequency, urgency, blood in urine, and nocturia [2] (Table 1).
The problem is that an enlarged prostate can obstruct the flow of urine through the urethra. Therefore, urination becomes increasingly difficult, and the bladder never feels wholly emptied. If the condition is left untreated, continued enlargement of the prostate transition zone eventually obstructs the urethra completely, and emergency measures become necessary to empty the bladder. Sonographically, BPH will show an expansion of the transition zone (TZ), and it can lead to hypoechoic areas within the prostate, calcifications, inhomogeneity, and cystic changes [3].
While a large body of literature exists regarding the impact of an enlarged prostate, less is known about the role of PVR, PV, and TRUS in the diagnostic evaluation of bladder obstruction and benign prostatic hyperplasia. However, to the best of my knowledge, no case report has assessed the significance of post-void residual urine, abdominal prostate ultrasound and transrectal prostate ultrasound in the sonographic evaluation of an enlarged prostate. Therefore, this case study is unique in many urological clinical aspects. Some researchers express caution towards using PVR measurements by transabdominal ultrasound, others referred to it as merely imprecise [4]. The hypothesis, however, is that ultrasound technology is a diagnostic tool used to detect an enlarged prostate gland. Therefore, this case report outlines the prognostic value of PVR, PV, and TRUS in the sonographic evaluation of an enlarged prostate.
Sonographic case report
Clinical History: The patient is a 62-year-old male, a married father of four children who present to the ultrasound department for evaluation of difficulty urinating (Table 2). According to the patient, the onset of the urinary symptoms has been gradual and have been occurring in a persistent pattern for months. Upon further interrogation, the patient describes the symptoms as frequent and nocturia but constant. The symptoms are associated with diabetes. However, patient denies having bladder cancer, hematuria, penile lesion, penile trauma or urethritis. There has been no associated bone pain, groin pain, hematospermia, pain with ejaculation, penile pain, perineal pain or scrotal pain. There is no history of previous surgery. The past medical history does not include chronic pelvic pain syndrome, urinary tract infection, radiation or high blood pressure. He was not a smoker but claimed to be a social drinker.
Diagnostic tests include prostate-specific antigen (PSA) testing. The testing reveals elevated PSA. The PSA was not drawn within 24 hours of ejaculation. According to the medical records, the patient has a history of an elevated PSA less than one year ago. The patient has not had a prostate biopsy, and there is no family history of prostate cancer. A registered nurse drew the blood for PSA blood testing.
Materials and Methods
This study was a case report performed at a urologic ultrasound department. A pelvic sonogram was ordered to assess post-void residual urine volume as well as transabdominal and transrectal ultrasound without biopsy (TRUS) to rule out an enlarged prostate. The patient had three ultrasound examinations: Urinary bladder ultrasound immediately after voiding in a uroflow machine; abdominal prostate ultrasound and transrectal prostate ultrasound. The bladder ultrasound and abdominal prostate ultrasound examination were performed with GE Logiq ultrasound machine with a 3.5 MHZ curved array transducer. The transrectal prostate examination was also performed with GE Logiq ultrasound machine with a 6.5 transrectal probe.
During the examination, sagittal and transverse scanning planes were obtained using gray-scale imaging. The patient was placed in a supine position during bladder and transabdominal prostate ultrasound examination and a left lateral decubitus (LLD) position during TRUS examination of the prostate.
Physical Exam: Vital signs: temperature, 98.5F; heart rate, 65 beats per minute; blood pressure: 122/80mm Hg; and respiratory rate, 18 breaths per minute. Labs: urine red blood cell count, 5 to 10 per high-power field; otherwise, complete blood count, comprehensive metabolic panel, and lipase were unremarkable. A licensed laboratory technician performed the lab test including the PSA serum laboratory test.
Chart Review: Patient information including demographics (age, sex, marital status) and medical data (vital sign, PSA levels, Lab results) was obtained by PACS chart.
>Sonographic Appearances:> Sonographically, the prostate gland is grossly enlarged, diffuse and heterogeneous. The paired seminal vesicles (SV) are hypoechoic and irregularly shaped. The bladder lumen is anechoic with the prostate gland indenting the base of the bladder obstructing the flow of urine. A registered sonographer performed the ultrasound examination.
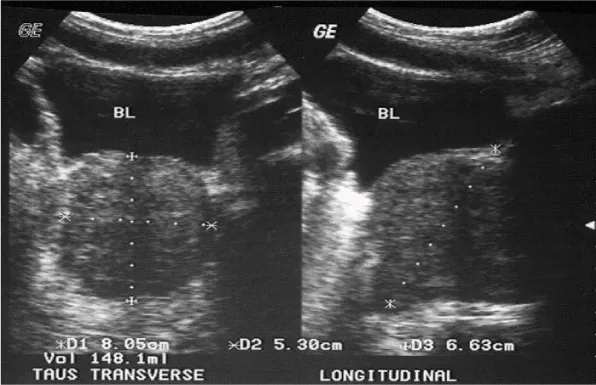
>Sonographic Analysis:> Three orthogonal diameters were obtained on each ultrasound measurements. On the longitudinal images, the longitudinal (DI=L) were measured on each of the images (i, e., PVR, PV, and TRUS). Transverse diameter (D2=W) and height (D3=H) were obtained during transverse imaging on each of the images (i.e., PVR, PV, and TRUS). These variables (VI, V2, and V3) were considered in estimating the actual urine residual and prostate volume. All variables including prostate and bladder volume were measured in centimeter (cm) and (ml) and used to assess the statistical significance of differences in mean quantitative ultrasound measurement between PVR bladder ultrasound, abdominal and transrectal prostate ultrasound (Table 2).
>Literature Search Strategy:> Literature review on the prognostic value of PV, PVR, and TRUS on the clinical outcome of BPH began with Internet searches at credible sites. Secondary sources led to primary sources. Recommended books on the topic were reviewed. This reading laid the foundation and understanding of the concepts of bladder ultrasound and BPH. Original scholarly research began at the Queens Library, NY using the EBSCO host for the databases including CINAHL, Health Sources, PsycINFO, Psych ARTICLES, Academic Search Premier, and Medline. The search was updated in March 2018. The references to all relevant studies were searched to identify any additional studies. Additionally, a systematic search of these computerized databases was conducted using the following keywords: transrectal ultrasound, prostate volume, bladder outlet obstruction, enlarged prostate and, post-void residual urine volume.
>Descriptive Epidemiology:> According to the literature, age is a significant risk factor in the development of an enlarged prostate gland [5]. BPH is common around the age of 40 or 50. The incidence rate of BPH increase per decade by 10%. By 80 years, the incidence will reach 80%. As such it is often thought of as a ‘normal’ part of aging. Despite the influence of age in the development of an enlarged prostate, hormonal and inflammation have been cited as a possible risk factor [5]. Also, epidemiological studies show an association between BPH and diabetes (Boon, Van Venrooij & Eckhardt, 2001). Also, Trumbeckas et al. [6], noted that enlargement of the prostate, bladder outlet obstruction and lower urinary tract symptoms is the basic triad for clinical diagnosis of benign prostatic hyperplasia (BPH).
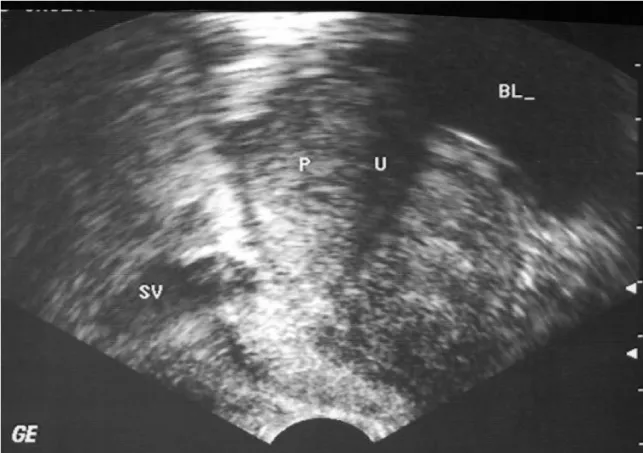
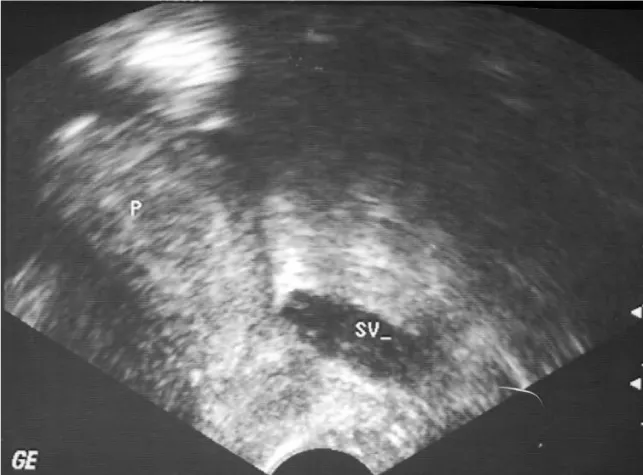
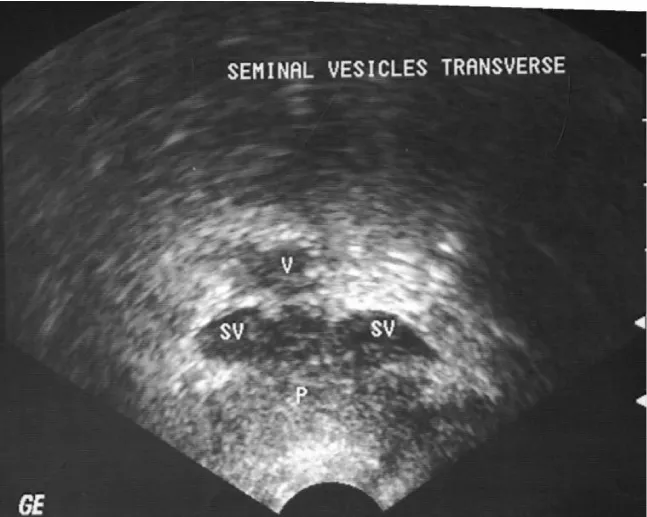
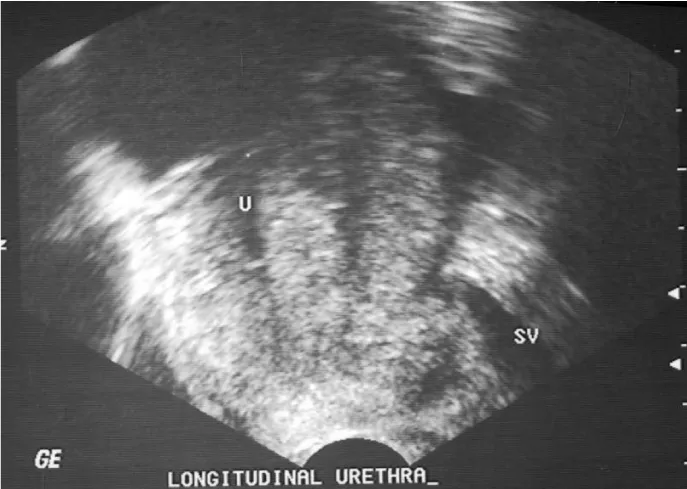
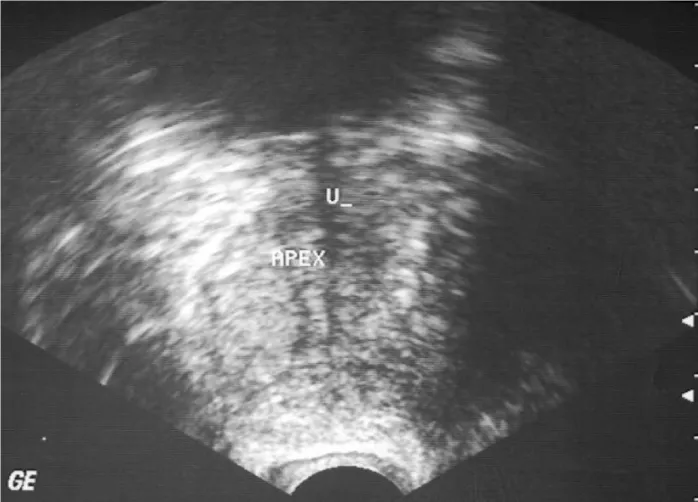
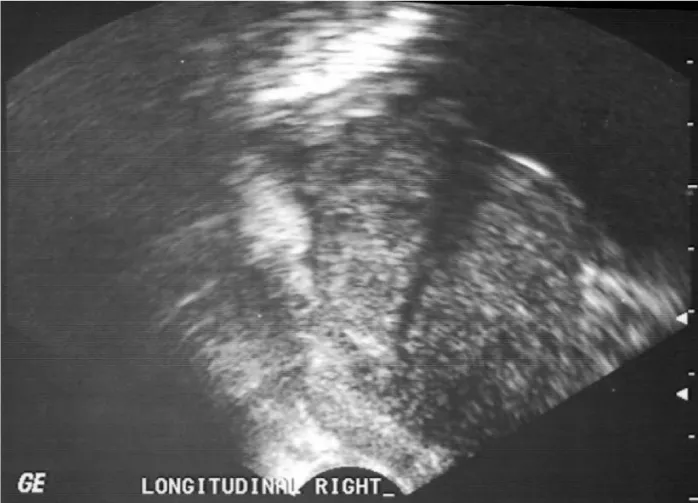
>Transrectal Prostate Ultrasound:> When performing a transrectal ultrasound of the prostate, the sonographers inverts the images seen on the screen. This convention allows the prostate anatomy to be seen in the natural anatomical orientation with anterior aspect on top of the screen, and the patient head to the left of the screen in the transverse view (Figures 1-11). The transrectal ultrasound of the prostate measures the prostate volume (PV) with the patient in a left lateral decubitus (LLD) position. In this procedure, a probe is inserted into the rectum to direct sound waves at the prostate. Sonographers use gray-scale ultrasound technology to take systematic images looking for an enlargement of the TZ. Sonographers take prostate images ranging from the apex, base and the longitudinal sections including the seminal vesicles (SV) and vas deferens (V) (Odwin & Fleischer, 2012).
According to the American Institute of Ultrasound in Medicine(AIUM), prostate gland volume measurements are taken both in coronal and longitudinal views from the apex to the base (volume=length x height x width x 0.52). The protocols for prostate imaging are presented in table 3. The seminal vesicles are also measured for size, shape, and symmetry. Sonographically, seminal vesicles are visualized as irregularly shaped and symmetrically paired structures and, the prostate (P) as a homogeneous gland with low-level echoes (Odwin & Fleischer, 2012). Any abnormalities in size and shape visualized on ultrasound are documented based on established departmental protocol. BPH will show an enlargement of the inner gland, may lead to hypoechoic areas within the gland and shows some levels of calcifications within the gland. An enlarged prostate gland may be diffusely heterogeneous with some cystic change.
>Transabdominal Prostate Ultrasound: The abdominal prostate ultrasound measures the PV with the patient in a supine position (Figure 12). However, the transabdominal approach is limited due to poor resolution of low-frequency transducers but useful for measuring prostate volume. Patients are advised to have a full bladder for transabdominal prostate ultrasound examination. Boo et al. [7], found that transabdominal ultrasound scanning is safe, convenient and has a definite value in the assessment of prostatic size.
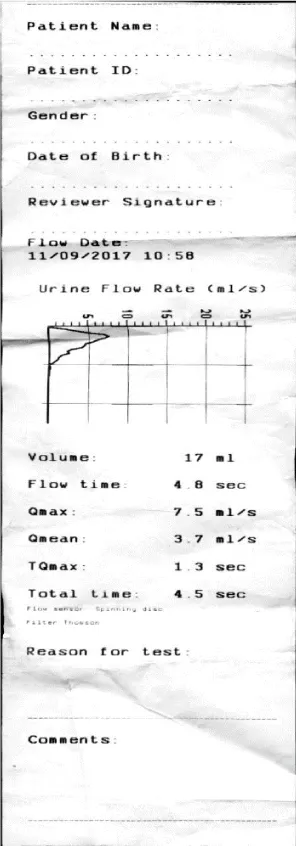
>Bladder Ultrasound: A distended bladder is necessary for sonographic evaluation of the bladder [8]. The doctor will ask a patient to urinate into a particular device that measures how quickly the urine is flowing. The device measures the flow and volume of the urine. A reduced flow often suggests BPH (Figure 13). The post-void bladder is then imaged with an ultrasound machine to record the urine residual in both longitudinal and transverse plane. Ultrasonography can show urine volume after micturition. Post-void residual (PVR) urine volume is the volume remaining in the bladder immediately after completion of voiding (Figure 14). Sonographically, the normal bladder appears cystic without internal echoes. The bladder wall should be well-defined, smooth contours and should not measure higher than about 3 mm when the bladder is fully distended. The probe should be angled from right to left to view the entire bladder. For the longitudinal view of the bladder, the transducer should be placed at the symphysis pubis at the midline. For the transverse view of the bladder, the transducer should be angled inferiorly, then superiorly at midline to view the entire bladder. In an adult, a residual value of less than 20 ml of urine is considered normal [8].
>Conventional Anatomy: The prostate gland is an encapsulated, fibromuscular and glandular organ located inferior to the neck of the bladder, anterior to the rectum and posterior to the symphysis surrounding the urethra. The gland is bordered laterally by the Levator Ani, and the Obturator Internus muscles. The prostate gland is part of the male reproductive system. By zonal anatomic convention described by McNeal [9], the prostate gland is divided into three glandular zones: (1) Peripheral zone (PZ); (2) Central Zone (CZ); (3) Transition zone (TZ) and, one nongranular, the anterior Fibromuscular Stroma (FS). According to McNeal [9], the PZ constitutes about 70 % of the gland and, is located posteriorly and laterally with 80 % of prostate cancer (PCa) originating from the zone. The CZ surrounds the ejaculatory ducts and anterior to the TZ. This zone constitutes about 20% of the gland. The CZ is located at the base of the prostate gland (Odwin & Fleischer, 2012). The TZ represents about 10% of the glandular tissues [10]. Various studies show that the TZ volume is directly associated with urodynamic obstruction of the bladder and it is a significant predictor of surgical outcome [11]. It is the site of Benign Prostatic Hypertrophy [10].
>Imaging Source: Ifeanyi Malu, RDMS. Legends: SV= Seminal Vesicle, V= Vas deferens, P = Prostate, U= Urethra, IPP= Intravesical prostatic protrusion.
Results
Transrectal ultrasound imaging of the prostate revealed an enlarged prostate gland measuring 7.25 X 5.02 X 6.58 with the volume of 86.8 ml (Table 1). The abdominal prostate volume (PV) is 148.1 ml. The intravesical prostate protrusion (IPP) showed an enlarged prostate gland indenting the bladder neck and measures 10.7 ml. The results show that an enlarged prostate and bladder disease may be evaluated using post-void residual urine measurement of the bladder, abdominal prostate ultrasound and evaluation of the prostate using the transrectal ultrasound method.
The uroflow machine recorded urine volume of 17 ml; mean is 3.7; QMax is 7.5 m/l and time of micturition is 4.8 second. TQmax is 1.3 ml/sec. The Flow Curve Pattern were interpreted as strain and obstructive. The volume of the ultrasound PVR bladder is 121.6 ml. The bladder lumen is anechoic. A transrectal sonogram showed an intravesical prostatic protrusion (IPP) and an enlarged prostate protruding inside the base of the bladder. The base of the prostate gland and TZ was noticeably enlarged. The outer gland, (i.e., the apex of the prostate gland) did not display hypoechoic or hyperechoic masses in the inferior segment. The patient was diagnosed with an enlarged prostate gland consistent with BPH.
Discussion
To the best of my knowledge, no case report has assessed the significance of post-void residual urine, abdominal prostate ultrasound and transrectal prostate ultrasound in the sonographic evaluation of an enlarged prostate. This case report examined the sonographic capabilities of PVR, PV and TRUS ultrasound images from a sonographers’ technical perspectives. Findings showed that these tools are significant in the diagnostic evaluation of patients presenting with an enlarged prostate and bladder obstruction. Although operators’ dependent, ultrasound technology has no post-procedure complications or radiation.
There is widespread accord in the literature that the size of the prostate gland increases throughout a man’s lifetime. The correlation between the size of the prostate gland and age is sufficiently proven in the literature. However, androgen and age have been traditionally considered the primary determinants of prostate enlargement( there is, however, an important role played by chronic inflammation in BPH pathogenesis). According to Amiel, Hollis & Ramasamy, (2016). BPH is a nonmalignant adenomatous overgrowth of the prostate gland with symptoms such as terminal dribbling, urinary retention and urges incontinence. The condition is one of the most frequent diagnoses leading to urology referral. BPH is not life-threatening. However, it significantly impacts patient quality of life. Many symptoms of an enlarged prostate stem from “obstruction of the urethra and gradual loss of bladder function, which results in incomplete emptying of the bladder.” Symptoms vary, but the most common ones involve changes or problems with urination, such as a hesitant, incomplete bladder emptying, straining, weak stream, urgency and leaking or dribbling, and urinary frequency, urgency, and nocturia [2].
There are many methods to treat an enlarged prostate. Transurethral resection of the prostate is a closed method preferred when there is minor enlargement of the gland and the patient is elderly and present a reduced surgical risk. Diagnosis of BPH is made by digital rectal examination, urine flow study and transrectal ultrasound. Cystoscopy is also used to diagnose an enlarged prostate. In this procedure, the doctor inserts a small tube through the opening of the urethra in the penis(eMedtv, 2006-2018). This test allows the doctor to determine the size of the gland and identify the location and degree of the obstruction. A Prostate Specific Antigen (PSA) Blood Test may be requested to rule out cancer as a cause of urinary symptoms.
The U.S. Food and Drug Administration approved a PSA test for use in “conjunction with a digital rectal exam to help detect prostate cancer in men age 50 or older and for monitoring prostate cancer patients after treatment”. However, research from the British Urological Association (2017) shows that PSA values can be used to examine cases of Benign Prostatic Hyperplasia (BPH) found mostly in the TZ of the prostate gland. PSA levels can be raised due to a range of conditions including BPH (British Urological Association, 2017; National Cancer Institute, 2012) ejaculation before PSA blood test [12] digital rectal examination [13] and, needle biopsy(Tchetgen, & Oesterling, 1997).
Amiel, Hollis & Ramasamy [2], noted that changes in the bladder, prostate, and urethra are associated with voiding dysfunction in the aging male. Another intriguing finding was that lower urinary infection might be caused by changes in the bladder such as bladder instability, decreased bladder compliance, and reduced bladder capacity. However, in our patient, these symptoms are due to BPH. With age, the prostate exhibits “glandular enlargement, increased smooth muscle tone and decreased compliance secondary to altered collagen deposition; these changes can lead to altered urinary symptoms due to outlet obstruction.” [2]. Our patient experienced urethral strictures and bladder neck contracture resulting in obstruction or blockage of urine passage. He was later diagnosed with BPH.
Singh and Kumar [14], noted that more men are destined to develop bothersome symptoms due to BPH. Furthermore, bladder wall thickness and post-void residual in conjunction with an intravesical prostatic protrusion(IPP) are “good predictors of clinically significant bladder outlet obstruction due to BPH,” [14]. IPP measurement for our patient is 10.7ml. In another study, [10] observed that uroflowmetry specifically QMax, can predict the natural history of the disease and a response to the surgery. Men with lower urinary tract symptoms (LUTS) and normal QMax is likely to have non-BPH related cause for their symptoms. Men with QMax of less than 10 ml/sec are more likely to have a urodynamic obstruction and may improve after surgery. According to Sundaram et al. [10], the most valuable parameter for prediction of obstruction is peak flow rate (QMax). If the QMax is more than 10 ml/sec, the obstruction is around 90%, and if the QMax is between 10-14 ml/sec then the obstacle is about 67% obstruction, and if the Qmax is more than 15 ml/sec, there is only 30% of obstruction.
In their study, Trumbeckas et al. [6], suggested that average/peak flow rate combined with total prostate volume can be used for prediction of obstruction. The authors noted that nearly 70% of men with peak flow rate (Qmax) less than 15 ml/s are obstructed. In our patient, the Qmax was 1.3 ml/sec. It has been proven by various studies that the diagnosis of obstruction of the bladder cannot be made by symptomatic assessment alone [6]. Therefore, Trumbeckas et al. confirmed that the best single predictor of blockage of the bladder is urinary flow rate. Trumbeckas et al. also noted that ultrasound estimated prostate weight or TZ volume could even predict obstruction.
In another study, Kelly [15], stated that uroflowmetry could serve as a noninvasive screening test for selecting patients who should undergo more sophisticated urodynamic studies (Figure 3). Although a patient with an enlarged prostate might lead to increased PVR volume following uroflowmetry, PVR measurement is significantly important in the diagnostic evaluation of a patient with symptoms indicative of an enlarged prostate [10].
In their seminal study, Yang et al. [16], enrolled 228 patients between the ages of 40 years and 64 years(at a mean age of 56.4 years) who underwent a transrectal prostate ultrasound. Yang et al. noted that despite the cost associated with transrectal ultrasound and the invasive nature of the procedure, PSA blood test, age, and urgency score are significant predictors of PV while transrectal prostate ultrasound (TRUS) was found to be a validated tool for PV estimation [16]. The authors found that the use of TRUS in PV estimation is significantly more precise and reproducible than the method of digital rectal examination which is less accurate especially for a patient with an enlarged prostate gland (PV > 25 mL) (Yang et al., 2016). These findings are consistent with results of a study by Boo et al. Boo and colleagues also postulated that ultrasound is a comfortable and safe way to measure the prostate size.
This case study remains limited by potential shortcoming. This was a single case study. Therefore, the findings cannot represent practice in all urologic critical care populations. A larger sample of all ages should be further investigated. However, this case and the images provided can be used as a baseline to which future case study of an enlarged prostate can be compared to evaluate the effectiveness of Ultrasound technology (UST).
In conclusion, sonographic post-void residual urinary volume(PVR) measurement has played a significant role in the evaluation of men with symptoms suggestive of benign prostatic hyperplasia(BPH) [17]. It is noninvasive, cost-effective and widely available. This case study showed similar diagnostic accuracy, suggesting that US is promising for future clinical diagnosis. Sundaram et al. also noted that men with symptoms suggestive of BPH should undergo clinical evaluation for prostatic size by trans-abdominal sonogram. They should further be evaluated by urine flowmetry for PVR urine to assess the severity of Bladder Outlet Obstruction (BOO). This case report make an essential contribution to the existing literature and can enhance positive social changes by providing an in-depth understanding of the diagnostic capabilities of UST in the evaluation of BPH [18,19].
Declaration of patient consent
The patient understands that name, and initial will not be published, and due efforts will be made to conceal identity. Financial support and sponsorship.
- Berry SJ, Coffey DS, Walsh PC, Ewing LL (1984) The development of human benign prostatic hyperplasia with age. Journal of Urology 132: 474-479. Link: https://tinyurl.com/y5xphze2
- Amiel G, Hollis M, Ramasamy R (2016) Medical Student Curriculum: BPH. Link:https://tinyurl.com/y5zf35y2
- Middleton W, Kurtz A, Hertzberg B (2004) Ultrasound: The Requisites. 2nd ed. St. Louis: Mosby 152-175.
- Simforoosh N, Dadkhah F, Hosseini SY (1997) The accuracy of residual urine measurement in men; comparisons between real-time ultrasonography and catheterization. Journal of Urology 158: 59-61. Link: https://tinyurl.com/y6xl9kcd
- Thompson TC, Yang G (2000) Regulation of apoptosis in prostatic disease. Prostatic Suppl 9: 25-28.
- Trumbeckas D, Milonas D, Jievaltas M, Matjosaiti J, kinciu M, et al. (2011) Importance of prostate volume and urinary flow rate in the prediction of bladder outlet obstruction in men with symptomatic benign prostatic hyperplasia. Central European Journal of urology 64: 75-79.Link: https://tinyurl.com/y32u9mc3
- Boo K, Ayob M, Salim M, Pahl C, Noori A, et al. (2012) Prostate volume ultrasonography. The relationship between body weight, height body mass index, and ethnicity in transabdominal measurement. Link: https://tinyurl.com/yym3d3qd
- Hagen-Ansert SL (2012) Textbook of Diagnostic Sonography. 7th Ed. Volume one. Elsevier: Mosby. St. Louis Missouri.
- McNeal JE (1968) Regional morphology and pathology of the prostate. American Journal of Clinical Pathology 49: 347-357.Link: https://tinyurl.com/y6s3yucy
- Sundaram D, Sankaran PK, Raghunath G, Vijayalakshmi S, Vijayakumar J, et al. (2017) Correlation of Prostate Gland Size and Uroflowmetry in Patients with Lower Urinary Tract Symptoms. Journal of Clinical and Diagnostic Research 11: AC01-AC04. Link: https://tinyurl.com/y6z2tk24
- Milonas D, Trumbeckas D, Juska P (2003) The importance of prostatic measuring by transrectal ultrasound in the surgical management of patients with clinically benign prostatic hyperplasia. Medicine 39: 860-866. Link: https://tinyurl.com/y5daz7sx
- Rajaei M, Momeni A, Kheiri S, Ghaheri H (2013) Effect of ejaculation on serum prostate-specific antigen level in screening and non-screening population. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences 18: 387-390. Link: https://tinyurl.com/y3vhmn5c
- The Internal Medicine Clinic Research Consortium (1995) Effect of digital rectal examination on serum prostate-specific antigen in a primary care setting. Archive of Internal Medicine 155: 389-392. Link: https://tinyurl.com/y3dr56de
- Singh I, Kumar S (2013) Does Intravesical Prostatic Protrusion Predict Bladder Outlet Obstruction in Patients with Lower Urinary Tract Symptoms Due to Benign Prostatic Hyperplasia? UroToday International Journal. Link: https://tinyurl.com/yxzwqvv7
- Kelly CE (2004) Evaluation of Voiding Dysfunction and Measurement of Bladder Volume. Reviews in Urology 6: S32–S37. Link: https://tinyurl.com/yymr8uz7
- Yang TK, Huang K, Chang H, Wang CW, Yang H (2012) Factors correlated with prostate volume in middle-aged men with bothersome lower urinary tract symptoms. Urological Science 27: 27-30. Link: https://tinyurl.com/y372exwn
- Bosch JL (1995) Postvoid residual urine in the evaluation of men with benign prostatic hyperplasia. World Journal of Urology 13: 17-20. Link: https://tinyurl.com/y257mccl
- Liu CC, Huang Li, WM (2007) The relationship between serum testosterone and measures of benign prostatic hyperplasia in aging men. Urology 70: 677-680. Link: https://tinyurl.com/yy7rqy2h
- Takahashi H, Ouchi T (1963) The ultrasonic diagnosis in the field of urology. Proc Japan Society of Ultrasonic Medicine 3: 7.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.






 Save to Mendeley
Save to Mendeley
