International Journal of Radiology and Radiation Oncology
A Prospective Study to Assess Radiation-Induced Dysphagia in Head and Neck Cancer Patients Treated with Dysphagia Optimized IMRT/VMAT Technique
1DNB Resident, Radiation Oncology, Caritas Hospital & Institute of Health Sciences, Kerala, India
2Senior Consultant, Radiation Oncology, Caritas Hospital & Institute of Health Sciences, Kerala, India
3Medical Physicist, Radiation Oncology, Caritas Hospital & Institute of Health Sciences, Kerala, India
4Biostatistician, Research and Development Cell, Caritas Hospital & Institute of Health Sciences, Kerala, India
5Research Associate, Public Health, Caritas Hospital & Institute of Health Sciences, Kerala, India
Author and article information
Cite this as
Kader SA, Joseph J, Aaron J, Joseph JK, Tom J, Joseph N, et al. A Prospective Study to Assess Radiation-Induced Dysphagia in Head and Neck Cancer Patients Treated with Dysphagia Optimized IMRT/VMAT Technique. Int J Radiol Radiat Oncol. 2025;11(1): 009-013. Available from: 10.17352/ijrro.000055
Copyright License
© 2025 Kader SA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Abstract
Background and objectives: Dysphagia is a common side effect of radiation therapy for head and neck cancers, significantly impacting patients’ physical, social, and emotional well-being. Validating efficient dysphagia-optimized radiotherapy techniques is crucial for improving health-related quality of life, a key determinant of curative management strategies. This study aims to analyze the clinical and functional outcomes following radical radiation in head and neck cancer patients using dysphagia-optimized radiation techniques.
Methods: This single-institution, prospective observational study assesses swallowing function clinically and using objective methods in patients with head and neck cancer treated with dysphagia-optimized IMRT/VMAT. The Dysphagia Aspiration-Related Structures (DARS) were delineated separately, with dose limits set by the DAHANCA guidelines. Clinical and objective assessments were conducted using ENT evaluation, clinical swallow study, UW QOL, and PSS HN questionnaires at 3- and 6-month intervals following radiation.
Results: Thirty-nine patients were enrolled, receiving either definitive or adjuvant radiation treatment with bilateral nodal irradiation. Significant differences in dysphagia were observed at 6 months post-radiation (p < 0.01). Grade 1 to 2 (CTCAE V 5.0) dysphagia was noted in most patients at 3 months post-RT, improving markedly by 6 months post-RT. All patients were disease-free at the 6-month follow-up, demonstrating effective local control and improved QOL with dysphagia-optimized IMRT/VMAT.
Conclusion: Using dysphagia-optimized IMRT/VMAT reduces the dose to DARS structures, enhancing the quality of life for patients undergoing definitive or adjuvant radiation therapy for head and neck malignancies without compromising local tumor control.
Introduction
Radical radiation therapy remains the mainstay of treatment in head and neck cancers, both in the primary as well as in the post-operative settings [1]. The addition of concurrent chemotherapy was proven to improve both local control and overall survival. Thus, concurrent chemo radiation given at doses of 66-70Gy in 30-33 fractions has been proven to be effective in achieving complete tumor response in head and neck cancers and enables organ preservation [2]. However, delivery of such radical radiation doses is not without side effects owing to the complex anatomy of the head and neck region, where the tumor often lies in proximity to many critical structures like the brainstem, spinal cord, DARS, and parotid glands. Thus, improved disease control comes at the cost of increased toxicity [1,3]. The advent of IMRT (Intensity modulated Radiation Therapy) came as a breakthrough in conformal radiotherapy. IMRT has gained attraction in head and neck cancers due to its inherent ability to treat irregular and concave-shaped treatment volumes lying in close vicinity to the critical organs by achieving increased steep dose gradients between the tumor and OARS, along with highly conformal dose coverages [4,5]. Also, when compared to 3DCRT, IMRT was found ideal in head and neck cancers as it allows sculpting out the radiation doses to target volumes, allowing better control of dose distributions within the PTVs. It also allows for the Simultaneous Integrated Boost (SIB-IMRT) technique [6]. This avoids the need for sequential boosts, thereby producing superior dose distributions while using the same plan for the entire course of treatment. Thus, dose-intensified schedules along with normal organ sparing became possible with IMRT. Longer treatment time and need for increased monitor units were the limitations of IMRT, which were tackled by VMAT (Volumetric Modulated Arc Therapy), which delivered IMRT in a continuous arc motion of the gantry with simultaneous variations of dose rate, gantry speed, and MLC position [7]. VMAT thus resulted in faster treatment delivery along with decreased monitor units, decreasing inter- and intra-fraction movement. Radiotherapy-induced dysphagia is a major side effect in head and neck cancer patients undergoing radical radiation. Persistent dysphagia can lead to increased aspiration, which in turn leads to prolonged tube feeding, psychological disturbances, and a downward trend in health-related quality of life [8]. The DARS trial has shown that do-IMRT (Dysphagia Optimized IMRT/VMAT) has improved patient-reported swallowing rates when compared with S-IMRT. In this study, we aim to see whether using do-IMRT/VMAT can bring a significant difference in the quality of life of head and neck cancer patients by assessing their dysphagia post radiation using clinical and objective methods.
Materials and methods
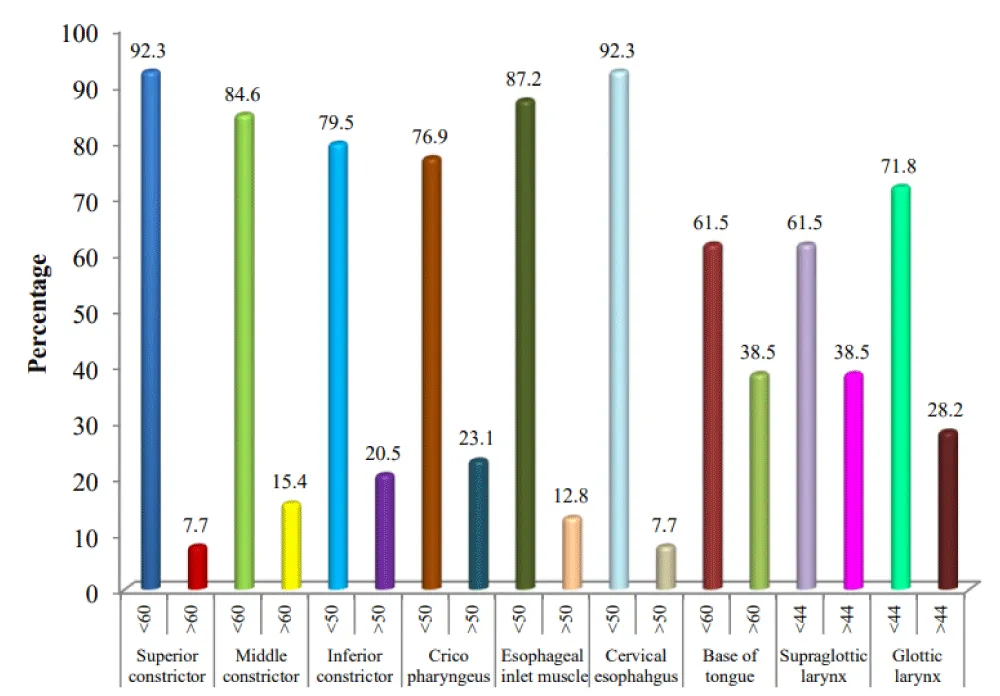
This single-arm prospective observational study assessed swallowing function in head and neck cancer patients treated with dysphagia-optimized IMRT/VMAT. No separate control group (eg, conventional IMRT or 3D CRT) was included. The study included 39 patients undergoing definitive or adjuvant radiation therapy targeting the tumor site and bilateral nodal areas. Swallowing function was evaluated clinically and objectively using ENT evaluations, clinical swallow studies, the UW-QOL (University of Washington Quality of Life) questionnaire, and the PSS-HN (Performance Status Scale for Head and Neck Cancer) questionnaire at 3 months and 6 months post-radiation. UW-QOL is a patient-reported outcome measure evaluating 12 domains, including pain, appearance, activity, recreation, swallowing, chewing, speech, taste, saliva, mood, and anxiety. PSS-HN is a clinician-rated scale assessing normalcy of diet, public eating, and understandability of speech. Both tools have been widely used to evaluate post-treatment functional outcomes in head and neck cancer patients and are sensitive to swallowing-related changes over time. In the dysphagia-optimized IMRT technique, Dysphagia Aspiration-Related Structures (DARS) were delineated with doses maintained within DAHANCA guidelines. Key structures included the superior, middle, and inferior constrictors, cricopharyngeus, esophageal inlet muscle, cervical esophagus, supraglottic and glottic larynx, and the base of the tongue. Dose constraints were ≤60 Gy for the superior and middle constrictors, ≤50 Gy for the inferior constrictor, cricopharyngeus, and esophageal inlet muscle, and ≤44 Gy for the supraglottic and glottic larynx.
Since there was no control group, we did a contextual comparison with historical controls from published literature in reference to baseline characteristics of patients enrolled in this study and outcomes for patients treated with conventional IMRT in similar settings.
Patients were immobilized using thermoplastic masks, with planning CT and fused MRI scans for better tumor delineation. Radiation doses included 66-70 Gy in 30-33 fractions to the high-risk PTV, 60 - 59.4 Gy to the intermediate-risk PTV, and 54 Gy to the low-risk PTV. Concurrent chemotherapy with Cisplatin at 40 mg/m² was administered unless contraindicated. Functional grading of dysphagia followed the CTCAE v5.0 criteria. Statistical analyses used repeated measure ANOVA, Friedman Test, Wilcoxon Signed Rank Test, and Fisher’s exact test, with p < 0.05 considered significant. Data were analyzed using SPSS version 20.0.
Results
A total of 39 patients were enrolled in the study. All patients underwent either definitive or adjuvant radiation treatment to the tumor site along with bilateral nodal irradiation. A median age of 57 years (range: 38-78 years). The majority of patients (80%) had locally advanced illness. The subsites included oral cavity (56.4%), oropharynx (17.9%), larynx (15.4%), and hypopharynx and nasopharynx together, less than 10%. Ten months was the median follow-up period (range: six to eighteen months). Baseline characteristics of patients are given in Table 1.
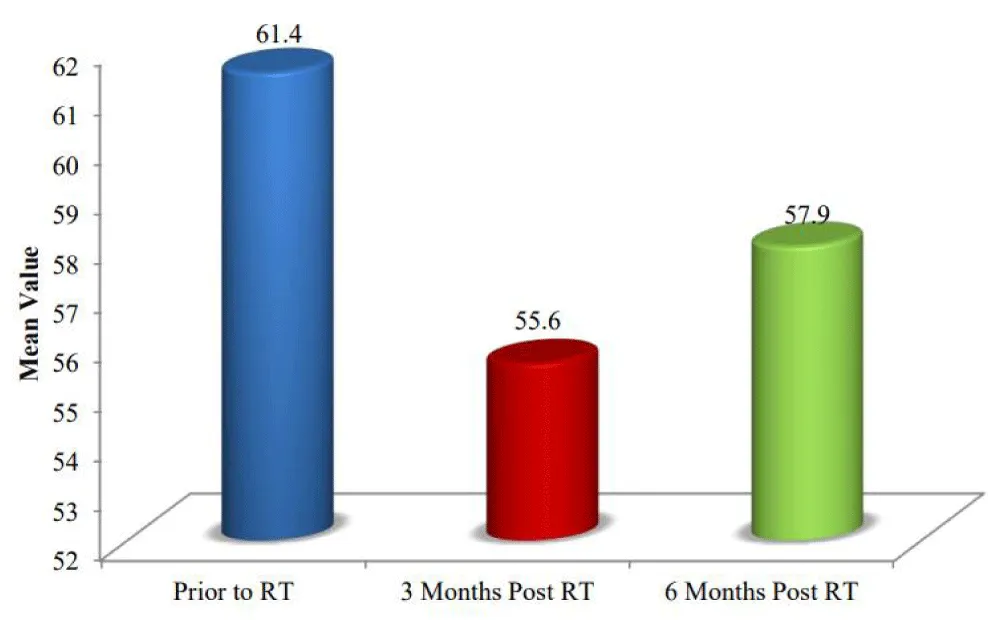
Patient weight monitoring is a simple but very effective method of monitoring dysphagia or feeding problems in head and neck cancer patients. There is a significant correlation between initial weight and weight at 3 months, while it is reaching pre-treatment weight at 6 months. The mean value of weight in kg at baseline is 61.4, which decreases to 55.6 at 3 months post-RT, and then slightly increases to 57.9 at 6 months post-RT, indicating a trend of initial decline followed by partial recovery (Figure 1). To maintain nutrition, all patients had either an NG tube or a PEG tube starting from the 2nd week of radiation till 6 weeks post RT.
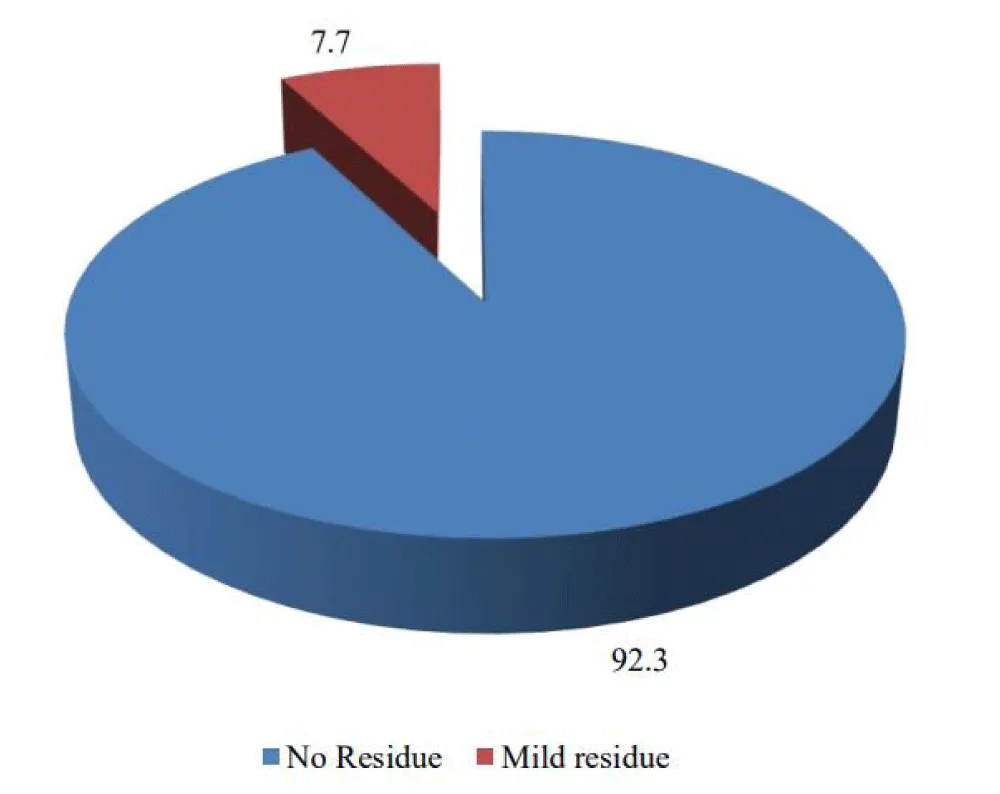
FEES study (done at 6 months post-RT), which looks at the presence or absence of food residue, showed 92.3% of subjects showing no residue and 7.7% showing mild residue. This highlights that the majority of subjects did not experience significant residue accumulation post-RT.
The important muscular regions of the swallowing apparatus received varying degrees of radiation doses. For each site, two categories are depicted: less than and greater than specific dose thresholds. The superior constrictor shows the highest percentage (92.3%) of subjects receiving less than 60 Gy and a small percentage (7.7%) receiving more than 60 Gy (Figure 2). Notably, the esophageal inlet muscle has a higher percentage (87.2%) of subjects receiving less than 50 Gy, while the cervical esophagus has a high percentage (92.3%) for less than 50 Gy, and the glottic larynx shows a significant distribution with 71.8% receiving less than 44 Gy (Figure 3). Other sites, such as the middle constrictor, inferior constrictor, cricopharyngeus, esophageal inlet muscle, cervical esophagus, base of tongue, supraglottic larynx, and glottic larynx, show varying distributions across the different dose categories.
Patient-reported outcomes were done using PSS HN and UWQOL, out of which significant domains are discussed here. Patient-reported outcome of swallowing at different stages post radiotherapy (RT) treatment was assessed by UWQOL. The swallowing domain included four questions, which were given points in a Likert scale model. 4-I can swallow as ever, 3-I cannot swallow certain solid foods, 2-I can only swallow liquid food, 1-I cannot swallow because it chokes me. It was assessed 3 months post-RT and 6 months post-RT. 41% of patients could only take liquids or pureed foods 3 months post RT, whereas 6 months post RT, only 2.6% patients belonged to this category. The remaining patients could eat semisolids and solids. These results indicate an overall improvement in dysphagia over time (Table 2).
Patient-reported outcome of taste at different stages post radiotherapy (RT) is shown in Table 3. This domain of UWQOL was also graded in a Likert scale fashion. 4- I can taste food normally,3- I can taste most foods normally, 2-I can taste some foods, 1-I cannot taste any foods. Around 50% of patients could only taste some foods 3 months post RT, while 6 months post RT, 50 % of patients could taste most foods normally.
All patients were disease-free clinically and radiologically at 6 months follow up which in turn showed that effective local control was also achieved along with better QOL using dysphagia optimized IMRT/VMAT technique.
Discussion
This is a single-institution prospective observational study to assess the swallowing function clinically and by objective methods in head and neck cancer patients by using dysphagia optimized IMRT /VMAT without compromising the dose to the target. Dysphagia remains a challenging side effect of head and neck radiotherapy, often leading to long-term complications affecting patients’ health and well-being. The study found that there was significant dysphagia at 3 months post-radiation, and marked improvement was observed by 6 months, supporting the hypothesis that optimized radiation techniques facilitate recovery from acute dysphagia. This finding is consistent with previous research that highlights the advantages of IMRT and VMAT in minimizing dose to critical structures compared to traditional 3DCRT [9-11]. Dysphagia optimized IMRT is a type of planning technique used to spare the DARS structures, especially the pharyngeal constrictor muscles lying in the intermediate and low risk CTVs [9,12,13]. Out of the 39 patients, the majority were males and above 60 years old. All patients completed the 3 and 6-month follow-up. We utilized dysphagia optimized IMRTwhere DARS structures are separately delineated and the dose to each structure is tried to be kept within dose limits as set by DAHANCA guidelines, as several trials showed the benefit of reducing the mean dose to DARS structures has an immense effect on reducing dysphagia associated with head and neck irradiation [13,14]. Our study showed improved swallowing function observed in this study underscores the importance of these techniques in achieving better functional outcomes, which was similar to other studies [15-18]. The use of multiple assessment tools, including ENT evaluations, clinical swallow studies, and quality of life questionnaires (UW-QOL and PSS-HN), provided a comprehensive view of the treatment’s impact. The observed improvement in swallowing function and quality of life at 6 months aligns with findings from other studies that report enhanced patient outcomes with dysphagia-optimized radiotherapy [19-23]. The impact of radiation on taste can significantly affect patients’ nutritional intake and overall quality of life, reinforcing the importance of comprehensive care approaches that address both dysphagia and taste alterations.
Comparison with conventional IMRT
While this study did not include a separate control arm, the results can be meaningfully interpreted against published outcomes for conventional IMRT. Multiple studies, including the PARSPORT trial [4] and DARS trial [13], have demonstrated the advantages of intensity-modulated and dysphagia-optimized techniques in reducing doses to critical swallowing structures. Mathew, et al. [9] reported higher mean doses to the superior constrictor and more persistent grade 2–3 dysphagia at 3 months post-treatment in patients treated with conventional IMRT. In contrast, in our cohort, 92.3% of patients received <60 Gy to the superior constrictor, with most patients showing only grade 1 dysphagia at 3 months and near-complete recovery of swallowing function by 6 months (Table 4) summarizes comparisons between conventional IMRT from Mathew et al. and dysphagia optimised IMRT/VMAT used in our study. The findings are also consistent with DARS and PARSPORT trials, which demonstrated improved functional outcomes without compromising tumour control when swallowing structures were prioritized in IMRT planning.
Conclusion
This single-institution prospective observational study is limited by its sample size and lack of a control group. The short follow-up period (up to 6 months) may not capture long-term dysphagia outcomes. Additionally, while multiple assessment tools were used, subjective measures like patient-reported outcomes may introduce bias. Further multicenter studies with larger cohorts and longer follow-ups are needed to validate these findings and to assess broader applicability. This study concludes that dose to DARS structures can be reduced by using dysphagia optimized IMRT/VMAT, which in turn leads to better quality of life in patients undergoing radical radiation therapy for head and neck malignancies without compromising the tumor control.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgement
We thank the patients for their consent and participation. Our sincere gratitude goes to the Caritas Hospital & Institute of Health Sciences- Department of Radiation Oncology, as well as the Research and Development Cell at Caritas Hospital &Institute of Health Sciences, for their invaluable support and collaboration in this case study.
References
- Cognetti DM, Weber RS, Lai SY. Head and neck cancer: an evolving treatment paradigm. Cancer. 2008;113(7 Suppl):1911–32. Available from: https://doi.org/10.1002/cncr.23654
- Nguyen NP, Sallah S, Karlsson U, Antoine JE. Combined chemotherapy and radiation therapy for head and neck malignancies: quality of life issues. Cancer. 2002;94(4):1131–41. Available from: https://doi.org/10.1002/cncr.10257
- Ghosh G, Tallari R, Malviya A. Toxicity profile of IMRT vs. 3D-CRT in head and neck cancer: a retrospective study. J Clin Diagn Res. 2016;10(9):XC01–3. Available from: https://doi.org/10.7860/jcdr/2016/21457.8583
- Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomized controlled trial. Lancet Oncol. 2011;12(2):127–36. Available from: https://doi.org/10.1016/s1470-2045(10)70290-4
- Wang X, Eisbruch A. IMRT for head and neck cancer: reducing xerostomia and dysphagia. J Radiat Res. 2016;57(Suppl 1):i69–75. Available from: https://doi.org/10.1093/jrr/rrw047
- Studer G, Huguenin PU, Davis JB, Kunz G, Lütolf UM, Glanzmann C. IMRT using simultaneously integrated boost (SIB) in head and neck cancer patients. Radiat Oncol. 2006;1(1):7. Available from: https://doi.org/10.1186/1748-717x-1-7
- Mashhour K, Kamaleldin M, Hashem W. RapidArc vs conventional IMRT for head and neck cancer irradiation: is faster necessarily better? Asian Pac J Cancer Prev. 2018;19(1):207. Available from: https://doi.org/10.22034/apjcp.2018.19.1.207
- Bossola M, Antocicco M, Pepe G. Tube feeding in patients with head and neck cancer undergoing chemoradiotherapy: a systematic review. JPEN J Parenter Enteral Nutr. 2022;46(6):1258–69. Available from: https://doi.org/10.1002/jpen.2360
- Mathew JM, Mukherji A, Saxena SK, Vijayaraghavan N, Menon A, Sriharsha K, et al. Change in dysphagia and laryngeal function after radical radiotherapy in laryngopharyngeal malignancies—a prospective observational study. Rep Pract Oncol Radiother. 2021;26(5):655–63. Available from: https://doi.org/10.5603/rpor.a2021.0078
- Petkar I, Bhide S, Newbold K, Harrington K, Nutting C. Dysphagia-optimised intensity-modulated radiotherapy techniques in pharyngeal cancers: is anyone going to swallow it? Clin Oncol (R Coll Radiol). 2017;29(7):e110–8. Available from: https://doi.org/10.1016/j.clon.2017.02.002
- King SN, Dunlap NE, Tennant PA, Pitts T. Pathophysiology of radiation-induced dysphagia in head and neck cancer. Dysphagia. 2016;31(3):339–51. Available from: https://doi.org/10.1007/s00455-016-9710-1
- Agarwal Sr K, Kumar P, Kumar P, Garg A, Nigam J, NS S. Feasibility of achieving dose constraints for dysphagia aspiration-related structures and its clinical significance in intensity-modulated radiotherapy planning of head and neck cancer. Cureus. 2024;16(2). Available from: https://doi.org/10.7759/cureus.53769
- Petkar I, Rooney K, Roe JWG, Patterson JM, Bernstein D, Tyler JM, et al. DARS: a phase III randomized multicentre study of dysphagia-optimised intensity-modulated radiotherapy (Do-IMRT) versus standard intensity-modulated radiotherapy (S-IMRT) in head and neck cancer. BMC Cancer. 2016;16:770. Available from: https://doi.org/10.1186/s12885-016-2813-0
- Feng FY, Kim HM, Lyden TH, Haxer MJ, Worden FP, Feng M, et al. Intensity-modulated chemoradiotherapy aiming to reduce dysphagia in patients with oropharyngeal cancer: clinical and functional results. J Clin Oncol. 2010;28(16):2732–8. Available from: https://doi.org/10.1200/jco.2009.24.6199
- Batham S, Gupta S, Ghosh A, Gupta I, Johny D, Srivastava S, et al. Comparative study of dysphagia-optimized intensity modulated radiotherapy (Do-IMRT) and standard intensity modulated radiotherapy (S-IMRT) and its clinical correlation in head and neck cancer patients. Asian Pac J Cancer Prev. 2023;24(11):3697–704. Available from: https://doi.org/10.31557/apjcp.2023.24.11.3697
- Upadhyay P, Kumar P, Chauhan AK, Kumar P, Nigam J, S N. Comparison of dosimetric parameters in dysphagia aspiration-related structures and clinical correlation in head and neck cancer patients treated with radiotherapy. Cureus. 2022;14(7):e26765. Available from: https://doi.org/10.7759/cureus.26765
- Nuyts S. Improving functional outcomes for patients with head and neck cancer. Lancet Oncol. 2023;24(8):827–8. Available from: https://doi.org/10.1016/s1470-2045(23)00281-4
- Roe JWG, Carding PN, Dwivedi RC, Kazi RA, Rhys-Evans PH, Harrington KJ, et al. Swallowing outcomes following intensity modulated radiation therapy (IMRT) for head & neck cancer – a systematic review. Oral Oncol. 2010;46(10):727–33. Available from: https://doi.org/10.1016/j.oraloncology.2010.07.012
- Petersson K, Finizia C, Pauli N, Dotevall H, Tuomi L. A randomized controlled study evaluating the head-lift exercise in head and neck cancer patients with radiation-induced dysphagia: effect on swallowing function and health-related quality of life over 12 months. Eur Arch Otorhinolaryngol. 2023;280(12):5445–57. Available from: https://doi.org/10.1007/s00405-023-08183-7
- Calcuttawala A, Shinghal A, Budrukkar AN, Swain M, Murthy V, Laskar SG, et al. Can dysphagia aspiration related structures (DARS) be spared in patients with oropharyngeal cancers? Dosimetric evaluation in a prospective study of DARS optimized intensity modulated radiation therapy. J Cancer Res Ther. 2024;20(5):1499–506. Available from: https://doi.org/10.4103/jcrt.jcrt_166_23
- Gluck I, Feng FY, Lyden T, Haxer M, Worden F, Chepeha DB, et al. Evaluating and reporting dysphagia in trials of chemoirradiation for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2010;77(3):727–33. Available from: https://doi.org/10.1016/j.ijrobp.2009.05.049
- Grant SR, Hutcheson KA, Ye R, Garden AS, Morrison WH, Rosenthal DI, et al. Prospective longitudinal patient-reported outcomes of swallowing following intensity modulated proton therapy for oropharyngeal cancer. Radiother Oncol. 2020;148:133–9. Available from: https://doi.org/10.1016/j.radonc.2020.04.021
- Anderson NJ. Improving dysphagia quality of life outcomes in patients receiving head and neck radiotherapy (Doctoral dissertation, Monash University). Available from: https://www.monash.edu/medicine/spahc/radiography/research/higher-degree-research-graduates
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
