International Journal of Radiology and Radiation Oncology
Incidence of Incidental Findings on Pediatric Oncologic PET/CT
Indu Rekha Meesa1*, Joseph J. Junewick2 and Paul Shreve3
2Helen DeVos and Spectrum Health Hospitals, Advanced Radiology Services, PC, USA
3Spectrum Health Hospitals, Advanced Radiology Services, PC, USA
Cite this as
Meesa IR, Junewick JJ, Shreve P (2015) Incidence of Incidental Findings on Pediatric Oncologic PET/CT. Int J Radiol Radiat Oncol 1(1): 019-022. DOI: 10.17352/ijrro.000006The purpose of this study is to determine the incidence and significance of incidental findings on pediatric oncologic PET/CT. A retrospective analysis of all PET/CT scans obtained at Helen DeVos Children’s Hospital between 2004-2008 in pediatric oncology patients was performed. Specific data points for study including DOB, primary diagnosis, secondary diagnosis, treatment status (chemotherapy and radiation) and PET/CT findings were obtained. Studies were reviewed and findings confirmed with board certified Nuclear Medicine and Pediatric Radiologists. Total of 104 patients with various tumors/malignancies underwent 323 integrated PET/CT for staging or monitoring. Of these 104 patients, 71 (68%) had at least one incidental finding present on the PET/CT and 116 of 323 (36%) studies had at least 1 incidental CT finding. In conclusion, our retrospective study shows that careful evaluation of especially the CT component of integrated PET/CT scans provides clinically important information which may necessitate additional workup or treatment.
Significance
Determine the incidence and significance of incidental findings on pediatric oncologic PET/CT.
Introduction
PET with the glucose analog 18F-FDG is increasingly recognized as a powerful tool in evaluating patients with various malignant tumors [1-3]. Recently, combined PET and CT systems (PET/CT) have emerged as promising imaging modalities and are being more routinely used in clinical situations [4-6]. PET/CT offers routine precise fusion of metabolic PET images with high-quality CT images.
Routine PET combines information from emission scans obtained with F-FDG and from transmission scans obtained with germanium-68 or cesium-137 for attenuation correction. CT has been adapted as the transmission scan, and the adaptation has enabled acquisition of fused PET/CT images. The CT component of PET/CT is also whole-body CT, and abnormalities that can affect treatment decisions or warrant additional treatment may be present. Therefore, it is important that CT images be interpreted in addition to PET images.
The purpose of our study was to report the prevalence of abnormalities that do not show increased F-FDG uptake on the CT component of integrated PET/CT in pediatric oncology patients.
Materials and Methods
A retrospective analysis of consecutive PET/CT scans in pediatric oncology patients obtained at Helen DeVos Children’s Hospital between 2004–2008 was performed. A total of 104 pediatric patients with various tumors/malignancies underwent 323 integrated PET/CT scans for staging or monitoring during the study period.
The most important variables for this study are the malignancy type, treatment status, and other diagnoses.
Axial CT images from all of the PET/CT studies were reviewed on stand-alone Picture Archiving and Communications Systems (PACS) workstations and correlated with findings from the accompanying PET and fused PET/CT images. The studies were reviewed and the findings confirmed by a board certified Nuclear Medicine and Pediatric Radiologist. For each patient with an abnormality present on CT scans that did not show increased F-FDG uptake, details were recorded concerning the nature of the abnormality, the anatomic location, and any information from previous and subsequent imaging studies and from the medical notes.
All recorded findings were classified as being of major, moderate, or minor significance, corresponding to definitions previously used in similar studies [7-9].
Major significance
CT appearance was highly suspicious for an abnormality relevant to the immediate treatment of the patient (e.g., additional cancers, metastatic lesions, other abnormalities that necessitated prompt clinical assessment).
Moderate significance
Imaging appearances suggested clinically important disease but required further correlation with other clinical or imaging findings.
Minor significance
Imaging appearances did not suggest clinically important disease and did not require additional workup.
Results
A total of 104 (46 female, 58 male) pediatric patients with various tumors/malignancies underwent 323 integrated PET/CT scans for staging or monitoring during the study period.
Lymphoma (52) Osteosarcoma (7)
Rhabdomyosarcoma (7) Ewing Scarcoma (6)
Testicular cancer (3) Melanoma (4)
Wilms tumor (2) Myofibroma (3)
Glioma/Low grade glioma (1) Undifferentiated sarcoma (4)
Noonan’s syndrome (1) Castlemans syndrome (1)
Right chest mass/PNET (1) Thyroid carcinoma (1)
Epilepsy or intractable seizures with Leukemia (7)
Pheochromocytoma (2)
Undifferentiated metastatic renal cell carcinoma (1)
Low grade adenocarcinoma of the parotid gland (1)
71 (68.2%) had at least one finding present on the CT component of the studies that did not exhibit correlative F-FDG activity.
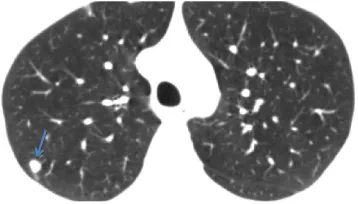
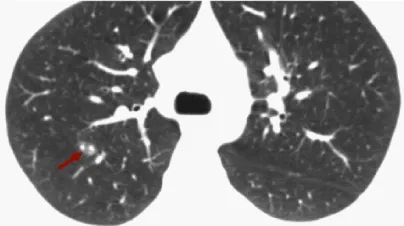
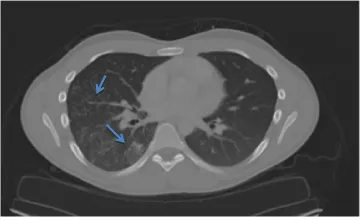
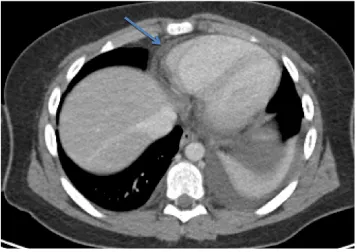
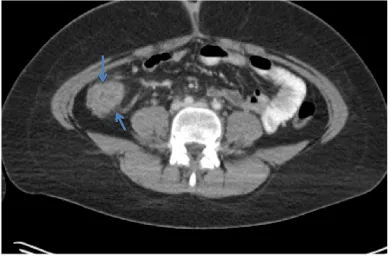
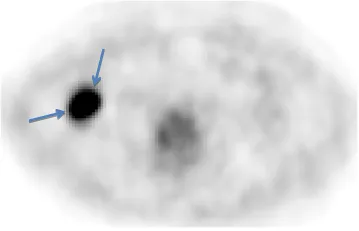
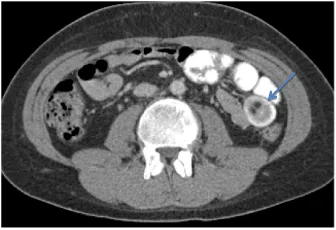
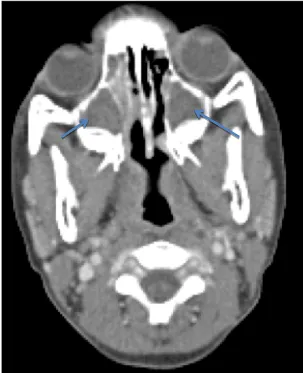
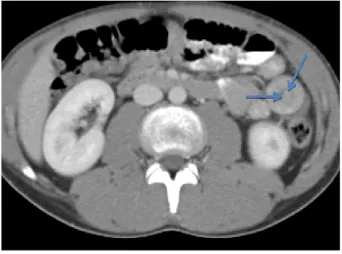
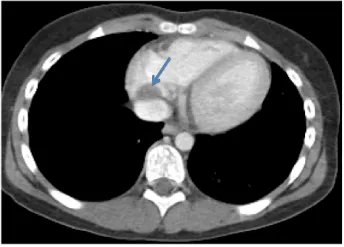
116 of 323 (35.9%) studies had incidental findings on CT, constituting a total of 128 abnormalities Tables 1-3, (Figures 1-8).
Location
Thorax (45)
Abdomen or pelvis (44)
Head and neck (29)
Bony skeleton (10)
Significance of findings
Major – 17/128 (13.3%)
Moderate – 73/128 (57%)
Minor – 38/128 (29.6%)
Discussion
The CT component of PET/CT, even if performed for purely anatomic localization, must be comprehensively interpreted to accurately identify all potentially important findings [9]. Evidence in our study shows that careful evaluation of the CT component of integrated PET/CT scans provides clinically important information. Our classification of abnormalities as being of major, moderate, or minor clinical importance, although somewhat subjective to the pediatric population, was used in an attempt to quantify the significance of abnormalities present on the PET/CT studies.
Some findings, such as transient intussusceptions, are unique to the pediatric population. Most cases of intussusceptions occurring between birth and five years of age are idiopathic. When intussusceptions develop in older children, it is usually due to what is known as a pathologic lead point. Meckel’s diverticulum and lymphoma are two classic examples of lead points. All three of the patients in our study with transient intussusceptions were older children with lymphoma.
In any patient with an underlying malignancy, there should be a heightened awareness to identify metastatic disease. Lymphoma, sarcoma, and testicular carcinoma, among others, have a high tendency to metastasize to the lungs. In our study, we had 15 patients with incidental pulmonary nodules on the CT thorax component of PET/CT. These nodules were identified and followed up closely on consequent PET/CT studies.
Most of our patients are in a hypercoagulable state due to their malignancy. A hypercoagulable prothrombotic state of malignancy occurs due to the ability of tumor cells to activate the coagulation system and it has been estimated that hypercoagulation accounts for a significant percentage of mortality and morbidity in cancer patients [10]. In our study, we identified 8 patients with a thrombus. Twelve patients were identified with renal hypodensities that could represent either simple cysts or small infarcts.
Oncology patients are also in an immunosuppressed state and their chances of acquiring an atypical infection is high. We identified a total of 15 patients with pneumonia and a total of 25 patients with paranasal sinus disease. Four patients had pleural effusions.
The CT component of PET/CT is also very useful for identifying radiation/chemotherapy induced changes. It is important to become aware of these changes so that these are not confused with tumor or reoccurrence of tumor. We had three patients with enteritis of colon, 3 patients with focal fatty liver, two patients with dermal changes (breast and buttocks), one patient with bladder wall thickening, and one patient with radiation induced changes in the brain, two patients with hydronephrosis, and one patient with pericardial effusion.
Finally, it is good to identify findings that are of minor clinical relevance because if symptoms due to these abnormalities develop, it is likely that the diagnosis will be reached more quickly if the presence of the abnormalities is known [11]. We identified 5 patients with spondylosis, 1 patient with a large lytic lesion in the inferior public ramus (likely an enchondroma), two patients with cholethiasis, one patient with a non-obstructive renal calculi.
Conclusion
Our retrospective study indicates that incidental findings are common and most had moderate or major significance. This establishes that PET/CT imaging is a very valuable tool for diagnosing additional pathology that may necessitate additional workup or treatment.
- Delbeke D (1999) Oncological applications of FDG PET imaging. J Nucl Med 40: 1706-1715.
- Gambhir SS, Czernin J, Schwimmer J, Silverman DH, Coleman RE, et al. (2001) A tabulated summary of the FDG PET literature. J Nucl Med 42: 1S-93S.
- Rohren EM, Turkington TG, Coleman RE (2004) Clinical applications of PET in oncology. Radiology 231: 305-332.
- Beyer T, Townsend DW, Brun T, Kinahan PE, Charron M, et al. (2000) A combined PET/CT scanner for clinical oncology. J Nucl Med 41: 1369-1379.
- Cohade C, Wahl RL (2003) Applications of positron emission tomography/computed tomography image fusion in clinical positron emission tomography: clinical use, interpretation methods, diagnostic improvements. Semin Nucl Med 33: 228-237.
- Von Schulthess GK, Steinert HC, Hany TF (2006) Integrated PET/CT: current applications and future directions. Radiology 238: 405-422.
- Hara AK, Johnson CD, MacCarty RL, Welch TJ (2000) Incidental extracolonic findings at CT colonography. Radiology 215: 353–357.
- Hellstrom M, Svensson MH, Lasson A (2004) Extracolonic and incidental findings on CT colonography (virtual colonoscopy). AJR 182: 631-638.
- Bar-Shalom R, Yefremov N, Guralnik L, Gaitini D, Frenkel A, et al. (2003) Clinical performance of PET/CT in evaluation of cancer: additional value for diagnostic imaging and patient management. J Nucl Med 44: 1200-1209.
- Caine CJ, Stonelake PS, Lip GY, Kehoe ST (2002) The Hypercoagulable State of Malignancy: Pathogenesis and Current Debate. Neoplasia 4: 465–473.
- Bruzzi JF1, Truong MT, Marom EM, Mawlawi O, Podoloff DA, et al. (2006) Incidental Findings on Integrated PET/CT That Do Not Accumulate F-FDG. AJR 187: 1116-23.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
