Global Journal of Cancer Therapy
Melanoma and basal cell carcinoma: Mimickers of each other
Gustavo de Sá Menezes Carvalho1*, Isabella N Dana2, Juliana Casagrande Tavoloni Braga1 and Ashfaq A Marghoob3
2Clinical Research Fellow, Memorial Sloan Kettering Cancer Center, New York, USA
3Dermatology service, Memorial Sloan Kettering Cancer Center, New York, USA
Cite this as
Sá Menezes Carvalho GD, Dana IN, Tavoloni Braga JC, Marghoob AA (2023) Melanoma and basal cell carcinoma: Mimickers of each other. Glob J Cancer Ther 9(1): 020-022. DOI: 10.17352/2581-5407.000051Copyright License
© 2023 Sá Menezes Carvalho GD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Basal cell carcinoma and malignant melanoma display unique dermoscopic features, at times they can mimic each other. A few clinical and dermoscopic algorithms, including the ABCD rule and the seven-point checklist, have been developed to simplify the diagnostic process. However, these tumors may present ambiguous dermoscopic patterns, lacking typical dermoscopic criteria. We present four cases where dermoscopic structures act as a confounding factor for the incorrect diagnosis of basal cell carcinoma and malignant melanoma. This work aims to improve the differentiation between melanoma and basal cell carcinoma. These tumors can sometimes be clinically similar and this can interfere with treatment if the correct diagnosis is not made.
Introduction
Dermoscopy has proven to increase the diagnostic accuracy of various skin tumors and differentiate benign from malignant tumors [1]. Although Basal Cell Carcinoma (BCC) and Malignant Melanoma (MM) display unique dermoscopic features, at times they can mimic each other [1-3]. Studies have analyzed the dermoscopic characteristics observed in atypical cases of BCC and MM, demonstrating that the atypical vascular pattern is a shared characteristic of these tumors and that the absence of pigmented structures can reduce diagnostic accuracy in these cases [4,5]. We present four cases where dermoscopic structures act as a confounding factor for the incorrect diagnosis of BCC and MM. These cases, as well as previous public cases [3,4], underscore that while BCC and MM may mimic each other, they will always reveal features concerning malignancy and lead to a biopsy.
Case reports
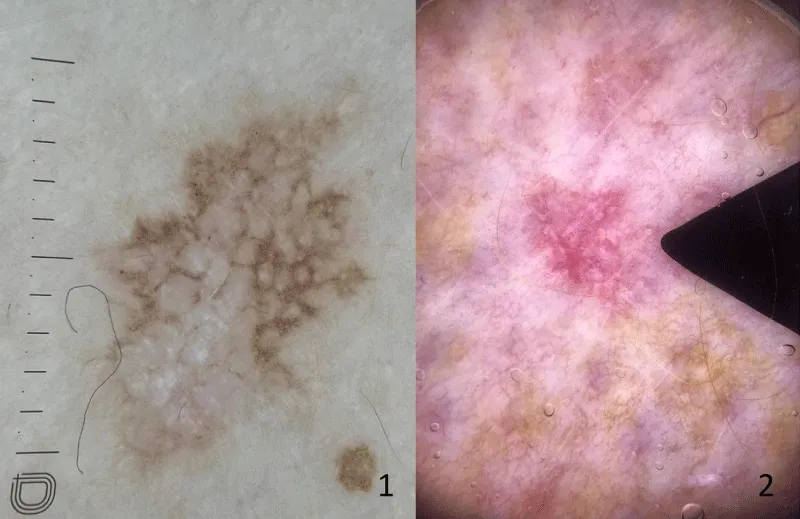
Case 1: A 68-year-old woman with a brownish lesion near her left knee for 2 years, with progressive growth. Dermoscopy showed angulated lines and bright white areas (Figure A1). According to these findings, the clinical diagnosis of extrafacial lentigo maligna was rendered and an excisional biopsy of the lesion was performed. The histopathological examination confirmed the diagnosis of superficial BCC and no features of a melanocytic lesion could be identified.
Case 2: A 62-year-old man with a papular lesion on the posterior region of the right leg that appeared 5 months ago. Dermoscopy showed a white-red structureless background, fine and well-focused vessels, and shiny white blotches and strands arranged throughout the lesion; structures compatible with the diagnosis of BCC (Figure A2). Histopathological examination, however, revealed a superficial spreading MM with Breslow 1.2mm, and no features of BCC were seen.
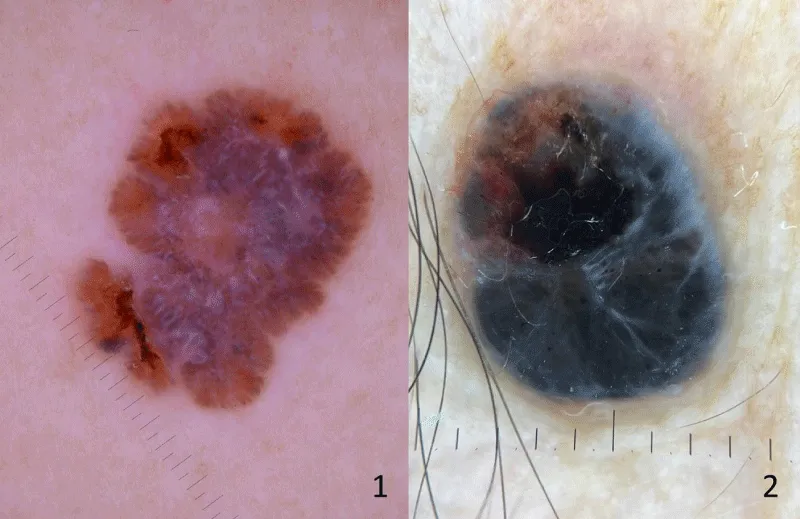
Case 3: A 59-year-old woman with a nodular and pigmented lesion in the right frontotemporal region with progressive growth for 4 months, with occasional bleeding. Dermoscopy showed a black-blue color pattern, bright white lines, atypical black dots, and ulceration (Figure B1); these findings suggested the diagnosis of pigmented nodular MM. Histopathological examination, on the other hand, showed a diagnosis of nodular pigmented BCC without any features of a melanocytic neoplasm.
Case 4: A 48-year-old woman with a pigmented lesion on her left arm that has been progressively growing for 2 years. Dermoscopy showed white shine lines and blotches, atypical streaks, a blue-white veil, and atypical vessels (Figure B2); these findings may be compatible with the diagnosis of MM. The histopathological diagnosis showed nodular and superficial BCC.
Discussion
Dermoscopy has greatly enhanced the accuracy of diagnosing BCC, with extensively described criteria showing high sensitivity and specificity [1]. Nevertheless, certain BCCs may display ambiguous dermoscopic patterns, lacking typical dermoscopic criteria, which can resemble other malignant skin tumors, like MM [3-6].
Most dermoscopic algorithms for diagnosing MM were established more than 20 years ago and the described criteria are an important tool for clinical practice [7,8]. A few algorithms, including the ABCD rule and the seven-point checklist, have been developed to simplify the diagnostic process [7,8]. These criteria are not, on the other hand, exclusive to MM [5-7], and can be found in other skin tumors such as BCC, such as those described here.
In the first case, the presence of well-demarcated angulated lines (straight lines that meet at angles larger than 90 degrees) [9] at dermoscopy was highly suggestive of lentigo maligna [2,9]. These criteria were later described for cases of pigmented BCC on the face mimicking lentigo maligna [6], but in other anatomical regions, it is quite rare. In the second case presented, there was the presence of atypical vessels, these criteria were described for atypical BCC in lower limbs [9-11]. However, even considering this atypical prerogative of dermoscopic presentation of this anatomical location, the present case was diagnosed as MM, showing that these observations are not universal.
In the third case was a predominant presence of the blue-black pattern, described primarily for pigmented nodular MM [12], however, pigmented BCC can mimic this clinical presentation in several anatomical areas, being more common in individuals with high phototype [3-5]. The fourth case had bright white areas and lines, a blue-white veil, and striae - structures associated with the diagnosis of MM. In these cases, reflectance confocal microscopy can be performed for diagnostic purposes, in addition to skin biopsy [3,13].
Conclusion
We described four cases where MM and BCC mimic each other, these cutaneous tumors may have common dermoscopic features and even in atypical cases, they may be present. This mimicry can lead to untimely clinical conduct, so the histopathological evaluation should always be considered first for the diagnosis and correct treatment of these cases.
- Puig S, Cecilia N, Malvehy J. Dermoscopic criteria and basal cell carcinoma. G Ital Dermatol Venereol. 2012 Apr;147(2):135-40. PMID: 22481576.
- Russo T, Piccolo V, Ferrara G, Agozzino M, Alfano R, Longo C, Argenziano G. Dermoscopy pathology correlation in melanoma. J Dermatol. 2017 May;44(5):507-514. doi: 10.1111/1346-8138.13629. PMID: 28447355.
- Peccerillo F, Mandel VD, Di Tullio F, Ciardo S, Chester J, Kaleci S, de Carvalho N, Del Duca E, Giannetti L, Mazzoni L, Nisticò SP, Stanganelli I, Pellacani G, Farnetani F. Lesions Mimicking Melanoma at Dermoscopy Confirmed Basal Cell Carcinoma: Evaluation with Reflectance Confocal Microscopy. Dermatology. 2019;235(1):35-44. doi: 10.1159/000493727. Epub 2018 Nov 7. PMID: 30404078.
- Di Matteo E, Pampena R, Pizzichetta MA, Cinotti E, Chester J, Kaleci S, Manfredini M, Guida S, Dika E, Moscarella E, Lallas A, Apalla Z, Argenziano G, Perrot JL, Tognetti L, Lai M, Cantisani C, Roberti V, Fiorani D, Baraldi C, Veneziano L, Papageorgiou C, Ciardo S, Rubegni P, Zalaudek I, Patrizi A, Longo C, Bianchi L, Pellacani G, Farnetani F. Unusual dermoscopic patterns of basal cell carcinoma mimicking melanoma. Exp Dermatol. 2022 Jun;31(6):890-898. doi: 10.1111/exd.14533. Epub 2022 Feb 6. PMID: 35102605; PMCID: PMC9305787.
- Pampena R, Lai M, Piana S, Pellacani G, Longo C. Basal cell carcinoma or melanoma, that is the question! J Eur Acad Dermatol Venereol. 2020 Aug;34(8):e425-e427. doi: 10.1111/jdv.16373. Epub 2020 Jun 1. PMID: 32180282.
- Navarrete-Dechent C, Uribe P, Rabinovitz H, Abarzua-Araya A, Kittler H. Basal Cell Carcinomas Presenting as Flat Pigmented Macules on the Face Mimicking Lentigo Maligna on Dermoscopy: A Case Series. Dermatol Pract Concept. 2023 Jan 1;13(1):e2023038. doi: 10.5826/dpc.1301a38. PMID: 36892346; PMCID: PMC9946124.
- Stolz W, Riemann A, Cognetta AB. ABCD rule of dermatoscopy: a new practical method for early recognition of malignant melanoma. Eur J Dermatol. 1994; 4:521–527.
- Argenziano G, Fabbrocini G, Carli P, De Giorgi V, Sammarco E, Delfino M. Epiluminescence microscopy for the diagnosis of doubtful melanocytic skin lesions. Comparison of the ABCD rule of dermatoscopy and a new 7-point checklist based on pattern analysis. Arch Dermatol. 1998 Dec;134(12):1563-70. doi: 10.1001/archderm.134.12.1563. PMID: 9875194.
- Vanden Daelen A, Ferreira I, Marot L, Tromme I. A Digital Dermoscopy Follow-up Illustration and a Histopathologic Correlation for Angulated Lines in Extrafacial Lentigo Maligna. JAMA Dermatol. 2016 Feb;152(2):200-3. doi: 10.1001/jamadermatol.2015.4132. PMID: 26651094.
- Bakos RM, Bakos L, Cartell A, Manzoni AP, Prati C. Radial streaking: unusual dermoscopic pattern in pigmented superficial basal cell carcinoma. J Eur Acad Dermatol Venereol. 2007 Oct;21(9):1263-5. doi: 10.1111/j.1468-3083.2007.02156.x. PMID: 17894724.
- Lombardi M, Pampena R, Borsari S, Bombonato C, Benati E, Pellacani G, Longo C. Dermoscopic Features of Basal Cell Carcinoma on the Lower Limbs: A Chameleon! Dermatology. 2017;233(6):482-488. doi: 10.1159/000487300. Epub 2018 Mar 22. PMID: 29566370.
- Argenziano G, Longo C, Cameron A, Cavicchini S, Gourhant JY, Lallas A, McColl I, Rosendahl C, Thomas L, Tiodorovic-Zivkovic D, Zaballos P, Zalaudek I. Blue-black rule: a simple dermoscopic clue to recognize pigmented nodular melanoma. Br J Dermatol. 2011 Dec;165(6):1251-5. doi: 10.1111/j.1365-2133.2011.10621.x. PMID: 21916885.
- Borsari S, Pampena R, Lallas A, Kyrgidis A, Moscarella E, Benati E, Raucci M, Pellacani G, Zalaudek I, Argenziano G, Longo C. Clinical Indications for Use of Reflectance Confocal Microscopy for Skin Cancer Diagnosis. JAMA Dermatol. 2016 Oct 1;152(10):1093-1098. doi: 10.1001/jamadermatol.2016.1188. PMID: 27580185.

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
