Global Journal of Cancer Therapy
Abrikossoff’s Tumour Mimicking a Neoplastic Tumour of the Breast: A Case Report
Alassiri A1*, Al Ali A1, Vaysse C1, Escourrou G2, Vinet B1 and Rimailho J1
2Anatomy-Pathology Service, iUCT, 1 av Irene Joliot Curie, 31100, Toulouse, France
Cite this as
Alassiri A, Ali A, Vaysse C, Escourrou G, Vinet B, et al. (2017) Abrikossoff’s Tumour Mimicking a Neoplastic Tumour of the Breast: A Case Report. Glob J Cancer Ther 3(1): 015-017. DOI: 10.17352/gjct.000016Introduction: Granular cell tumours (GCT), also known as Abrikossoff’s tumours, are rare, and occur in the breast in approximately 5-6% of the cases these tumours are usually benign with only 1% of malignancy.
Case Presentation: A 57-year-old Caucasian woman presented with a palpable mass that was growing progressively in the axillary tail of the left breast, with no other associated symptoms, and no family history of breast cancer.
Discussion: It is important that this type of lesion be identified clinically, radiologically and pathologically by all physicians managing breast tumours, in order to offer the most appropriate treatment. Using this classical clinical case, we will discuss the histological characteristics and the management of this type of lesion.
Conclusion: A biopsy of the lesion provided a definitive diagnosis, and a wide local incision was recommended as the treatment plan.
Case Presentation
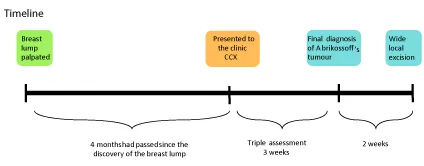
A 57-year-old Caucasian woman presented to our clinic with a palpable mass in the axillary tail of her left breast it had been growing progressively for 4 months, with no other associated symptoms. This patient had no family history of breast cancer, nor anything particular to this case in her medical history. Upon physical examination of the left breast, a 2 cm mass was palpable at 2 o’clock, tethered to the overlying skin (Figure 1). The mass was immobile, firmly attached to the skin and underlying tissue, and was not tender to the touch. The left nipple was not retracted, and there was no apparent discharge. There were no palpable axillary lymph nodes.
As part of the triple assessment, this patient underwent ultrasonography and mammography. Because these assessments showed non-contributory and clinico-radiological discordance, an MRI were performed, which found a 6 mm irregularly contoured lesion, enhanced in an unspecified manner. The mass was given a Breast Imaging Reporting and Data System (BI-RADS) score of 4 (following the scoring system of the American College of Radiology). This mass was suspected to be malignant, so a core biopsy was performed. The pathological examination of the biopsy revealed the proliferation of large cells, with abundant granular eosinophilic cytoplasm and a small central core stained positive for PS100, but negative for cytokeratin (Figure 2).
The triple assessment was concluded with a final diagnosis of Abrikossoff’s tumour, and a wide local excision was performed, as recommended by a review of the literature. A further pathological investigation confirmed the diagnosis. The margins were clear, and no further treatment was recommended.
Patient was seen in consultation in our outpatient clinic a month after discharge as postoperative follow. No further follow up was needed because of the benign findings of the lesion (Figure 3).
Discussion
GCTs are rare which commonly found in the head and neck of which more than 50% of the cases [1]. A GCT of the breast usually develops in premenopausal women, of AfricanAmerican ethnicity. Rarely found in adolescent age group. It presents clinically as malignant breast cancer usually with signs of tethering of the skin, infiltration and ulceration. This presentation corresponds to the Histological findings of GCTs which arises form interlobular breast stromal tissue and tend to form cords that extend into adjacent normal breast parenchyma, a characteristic that simulates the growth pattern of infiltrating carcinoma making it difficult to diagnose clinically and radiologicaly [2].
The origin of these tumours has long been discussed, and they tend to stain positive for the S-100 protein, which supports the hypothesis that they are derived from Schwann cells, which is found in peripheral nerves. In a study by Adeniran et al., a GCT was shown to be negative for oestrogen and progesterone [3]. With low mitotic levels. Other cases in the literature have shown negativity for cytokeratin, myoglobin, desmin, neurofilaments, glial fibrillary acidic protein (GFAP) and lysozyme. The ultrasonographic and mammographic presentations are variable, and a GCT can often be interpreted as a suspicious lesion, with neoplastic characteristics requiring an additional MRI (usually in the case of clinicalradiological discordance like we have faced in this case).
As mentioned before Granular cell tumours are known to be benign with good prognosis but 1 % of all GCTS are malignant [4,5]. Malignant features include: large size more than 4 cm, increased mitotic rate, rapid growth, local invasion, and variation in cell size and shape [6]. A bad prognosis is defined by the findings of histological malignancy leading to survival rate of a median interval of 3years [6].The most accepted histological criteria for diagnosing MGCTs were established by Fanburg-Smith, et al., [6]. (FS criteria). These researchers proposed the following six histological criteria for the selection of atypical or MGCTs in their study of 73 cases of GCTs: necrosis, spindling of the tumor cells, vesicular nuclei with large nucleoli, an increased mitotic rate [>2 mitoses/10 high-power fields (HPFs) at 200× magnification], a high nuclear-to-cytoplasmic ratio and pleomorphism. A GCT was classified as “malignant” if it had 3 or more of these features, “atypical” if it had only 1–2 features and “benign” if none of these features or a focal nuclear pleomorphism was present.
Throughout the literature, A core biopsy is recommended in order to rule out neoplasia. Based on this information, a wide local excision of the breast mass is the best treatment. No other treatments like chemotherapy or radiotherapy or a combination of both have been found useful to treat GCTs [2]. While the vast majority of GCTs of the breast are benign in nature, it is not considered realistic to treat all GCT cases with the surgical treatment or adjuvant therapy used for malignant ones.
Conclusion
This tumour-mimicking neoplasia cannot be diagnosed during the initial examination. A biopsy of the lesion provides a definitive diagnosis, and should be done prior to any management plan. Surgical treatment, with a wide local excision, is the recommended treatment plan for its malignant tendencies. However, there have been no particular or specific recommendations described about the subsequent follow up.
- Rosso R, Scelsi M, Carnevali L (2000) Granular cell traumatic neuroma: a lesion occurring in mastectomy scars. Arch Pathol Lab Med. May 124: 709-711. Link: https://goo.gl/Z6zWib
- Nicole DS, Allison A, Carla C (2011) Granular Cell Tumor of the Breast: Clinical and Pathologic Characteristics of a Rare Case in a 14-Year-Old Girl. J of Clinical Oncology 29:656–657. Link: https://goo.gl/M3Bm5h
- Adeniran A, Al-Ahmadie H, Mahoney MC, Robinson-Smith TM. (2004). Granular cell tumour of the breast: a series of 17 cases and review of the literature. Breast J 10: 528-531. Link: https://goo.gl/oFP9jO
- Chetty R, Kalan MR (1992) malignant granular cell tumour of the breast. J Surg Oncol 49: 135-137. Link: https://goo.gl/UFl1Nt
- Uzoaru I, Firfer B, Ray V, Hubbard SM, Rhee H (1992) malignant granular cell tumour. Arch Pathol Lab Med 116: 206-208. Link: https://goo.gl/A29Q8j
- Fanburg Smith JC, Meis Kindblom JM, Fante R, Kindblom LG (1998) malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. AM J Surg Pathol 22: 779-794. Link: https://goo.gl/TcrxAp
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
