International Journal of Immunotherapy and Cancer Research
Lymphoepithelioma like Carcinoma of the Bladder – “A Case” Revisited
Mezhuneituo Raleng1, Gaurav Aggarwal2* and Sujoy Gupta3
2MS, DNB (Urology), Fellowship (Surgical Oncology), Consultant, Uro-Oncology, Tata Medical Center, Newtown, Kolkata, West Bengal, India
3MS, FRCS, FRCS (Urology), Sr. Consultant, Uro-Oncology, Tata Medical Center, Newtown, Kolkata, West Bengal, India
Cite this as
Raleng M, Aggarwal G, Gupta S (2020) Lymphoepithelioma like Carcinoma of the Bladder – “A Case” Revisited. Int J Immunother Cancer Res 6(1): 019-021. DOI: 10.17352/2455-8591.000025Lymphoepitheliomas are a type of undifferentiated carcinomas primarily described in the nasopharyngeal cavity. In the urinary tract, they are typically, but uncommonly seen in the urinary bladder, although occasional cases have been reported in the renal pelvis, ureter and urethra. Lymphoepithelioma-like carcinoma of the urinary bladder, first reported by Zuckerberg, et al. in 1991, is uncommon with a reported incidence between 0.4 and 1.3% of all bladder carcinomas.
We report the case of an 82 year old gentleman, who presented with a bladder mass, which was post surgical intervention, diagnosed to be a Lymphioepitelioma like carcinoma, with an aim to add to the available literature, and help re-visit and establish appropriate treatment strategies.
Introduction
Lymphoepitheliomas are a type of undifferentiated carcinomas primarily described in the nasopharyngeal cavity. In the urinary tract, they are typically, but uncommonly seen in the urinary bladder, although occasional cases have been reported in the renal pelvis, ureter and urethra [1,2].
Lymphoepithelioma-like carcinoma of the urinary bladder, first reported by Zuckerberg, et al. in 1991, is uncommon with a reported incidence between 0.4 and 1.3% of all bladder carcinomas [1,2].
We report the case of an 82 year old gentleman, who presented with a bladder mass, which on post surgical histopathology examination was diagnosed to be a Lymphoepithelioma like carcinoma.
Case report
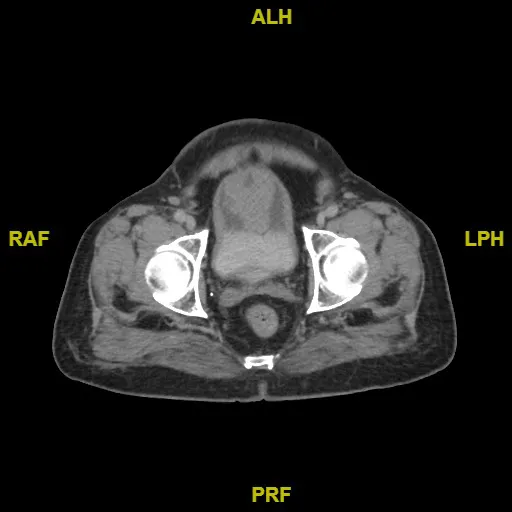
An 82 year old gentleman presented to our outpatient department, with intermittent hematuria and Lower Urinary Tract Symptoms (LUTS) since the last 2 months. He was an ex-smoker, a known hypothyroid and hypertensive patient. General clinical examination was unremarkable. A CT(Computed tomography) scan showed a 4.3 x 5.5 cm urinary bladder mass in the anterior wall (Figure 1) and all blood tests were within normal limits.
He was taken up for a standard trans-urethral resection of bladder tumor (TURBT). Intra-operatively, cystoscopy revealed a large, solid, vascular tumor arising from the dome of the bladder of approximate size 8 x 9 cm, corresponding with the CT images.
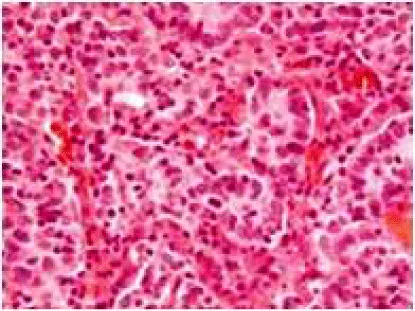
Post procedure-histopathology revealed a high grade invasive urothelial carcinoma, favouring lymphoepithelioma-like variant (Figure 2), extensive lamina propria invasion with deep muscle (detrusor) invasion, immunohistochemistry(IHC) was positive for cytokeratin (AE1/AE3) and negative for p63 and EBER-ISH (Ebstein Barr Virus Encoded RNA- In Situ Hybridisation). His case was put up through our institutional multi-disciplinary tumor-board (MDT) meeting and considering his age, co-morbidities (hypertension and hypothyroidism) as well as the morbidity/mortality associated with a radical cystectomy + urinary diversion, he was advised a partial cystectomy.
CT thorax and abdomen done post-TURBT, as a part of routine staging, revealed focal thickening and enhancement in the apex of bladder (up to 1.3 cm), with no lymphadenopathy or distant metastasis.
The partial cystectomy and bilateral pelvic lymph node dissection was performed without event and he was discharged on his 5th post operative day.
His final histopathology revealed a high grade invasive urothelial carcinoma, favoring lymphoepithelioma-like variant (70% lymphoepithelioma and 30% usual urothelial carcinoma). Tumour had infiltrated the perivesical fat microscopically and there was no nodal metastasis- giving the following staging: pT3aN0M0.
In lieu of his age, as well as caveats in literature as regards further management strategies, the MDT decided not to offer adjuvant chemotherapy and keep him on active surveillance.
A surveillance flexible cystoscopy at 1 year, post procedure was normal, along with no clinic-radiological evidence of recurrence.
Discussion
Lymphoepithelioma like tumors of the urinary bladder (LELCB) are a rare entity with an incidence of about 1% of all bladder tumors [1,2]. Due to this rarity, there are currently no standardized treatment guidelines for LELCB. It is commonly accepted that hematuria is the most common presenting feature [1,3]. Currently with the development of Immunohistochemistry (IHC), the diagnosis is much easier than it was in 1991 when it was first noticed [4] and it is known that LELCB is usually muscle invasive at diagnosis but not metastatic, as with other bladder cancers [5]. But there are reports that LELCB can occur in a background of Transitional Cell Carcinoma (TCC) and these behave more aggressively. Lopez, et al. in their series found that patients with LELCB in a background of high-grade TCC died of the disease 3–30 months from diagnosis [5].
Thus, presently there is still confusion regarding the long term aggressiveness of the disease and thus the role for adjuvant therapy is still debated. Generally they are considered sensitive to radiotherapy and chemotherapy [6,7], while some Japanese centers advocate adjuvant chemoradiotherapy [2].
Amin, et al. [8], have described a classification system, determined by the percentage of LELCB morphology within the tumor, characterising pure (100%), predominant (>50%) and focal (<50%) disease.
Williamson, et al. suggest that for pure or predominant LELCB a transurethral resection and adjuvant chemotherapy is adequate. [9] While Kozyrakis, et al. would prefer radiotherapy or radical cystectomy to high risk patients [3] Tamas in their series of 28 patients found that 47% of them were associated with urothelial cancers with high propensity for multifocality, so they favor radical cystectomy over partial cystectomy [10]. Procaro, et al. gives a reasonable suggestion of performing TURBT with or without chemotherapy for pure or predominant LELCB and radical surgery with chemotherapy for focal muscle invasive LELCB [7].
Since LELCB was initially described in the nasopharynx and has been associated with Epstein Barr virus, some authors suggest that one should exclude a primary tumor occurrence in the nasopharynx [3].
Conclusion
Lymphoepithelioma like carcinomas of the bladder are a clinical rarity, with no set management protocols. On account of this, reports of this disease re-visited, akin to ours, would help to add to the caveats in literature and help clinicians to plan appropriate treatment strategies.
- Yang AW, Pooli A, Lele SM, Kim IW, Davies JD, et al. (2017) Lymphoepithelioma-like, a variant of urothelial carcinoma of the urinary bladder: a case report and systematic review for optimal treatment modality for disease-free survival. BMC Urol 17. Available from: Link: https://bit.ly/3mkuNqT
- Yoshino T, Ohara S, Moriyama H (2014) Lymphoepithelioma-like carcinoma of the urinary bladder: a case report and review of the literature. BMC Res Notes 7. Link: https://bit.ly/33ijNl4
- Kozyrakis D, Petraki C, Prombonas I, Grigorakis A, Kanellis G, et al. (2011) Lymphoepithelioma‐like bladder cancer: Clincopathologic study of six cases. Int J Urol 18: 731-734. Link: https://bit.ly/2FdQ3xM
- Zukerberg LR, Harris NL, Young RH (1991) Carcinomas of the urinary bladder simulating malignant lymphoma. A report of five cases. Am J Surg Pathol 15: 569-576. Link: https://bit.ly/33kpVZV
- Lopez-Beltrán A, Luque RJ, Vicioso L, Anglada F, Requena MJ, et al. (2001) Lymphoepithelioma-like carcinoma of the urinary bladder: a clinicopathologic study of 13 cases. Virchows Arch Int J Pathol 438: 552–557. Link: https://bit.ly/2GLUFLH
- Amin MB, Ro JY, Lee KM, Ordóñez NG, Dinney CP, et al. (1994) Lymphoepithelioma-like carcinoma of the urinary bladder. Am J Surg Pathol 18: 466-473. Link: https://bit.ly/3m6vrYR
- Porcaro AB, Gilioli E, Migliorini F, Antoniolli SZ, Iannucci A, et al. (2003) Primary lymphoepithelioma-like carcinoma of the urinary bladder: report of one case with review and update of the literature after a pooled analysis of 43 patients. Int Urol Nephrol 35: 99–106. Link: https://bit.ly/3hnyzff
- Amin MB, Ro JY, Lee KM, Ordóñez NG, Dinney CP, et al. (1994) Lymphoepithelioma-like carcinoma of the urinary bladder. Am J Surg Pathol 18: 466-473. Link: https://bit.ly/3m6vrYR
- Williamson SR, Zhang S, Lopez-Beltran A, Shah RB, Montironi R, et al. (2011) Lymphoepithelioma-like carcinoma of the urinary bladder: clinicopathologic, immunohistochemical, and molecular features. Am J Surg Pathol 35: 474-483. Link: https://bit.ly/3ip9lP4
- Tamas EF, Nielsen ME, Schoenberg MP, Epstein JI (2007) Lymphoepithelioma-like carcinoma of the urinary tract: a clinicopathological study of 30 pure and mixed cases. Mod Pathol 20: 828-834. Link: https://bit.ly/3mbB4VB
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
