International Journal of Immunotherapy and Cancer Research
Analysis of Risk Factors for Development of Hepatocellular Carcinoma in Chronic HBV - Infected Liver Cirrhosis Patients: A Meta-Analysis
Xiang Lyu1†, Gaofeng Cai2†, Kui Liu3†, Sichao Huang3, Jun Yao2, Zhenggang Jiang2, Zhengting Wang2, Zhifang Wang2*, Yongdi Chen2*, Huakun Lv2* and Jianmin Jiang2*
2Zhejiang Provincial Center for Disease Control and Prevention, 3399 Binsheng Road, Hangzhou 310051, China
3Medicine School, Ningbo University, 818 Fenghua Road, Ningbo 315000, China
†These authors contributed equally to this work
Yongdi Chen, Zhejiang Provincial Center for Disease Control and Prevention, 3399 Binsheng Road, Hangzhou 310051, Fax: +86-571-8711-5104, E-Mail: [email protected]
Huakun Lv, Zhejiang Provincial Center for Disease Control and Prevention, 3399 Binsheng Road, Hangzhou 310051, Tel: +86-571-8711-5133, E-Mail: [email protected]
Jianmin Jiang, Zhejiang Provincial Center for Disease Control and Prevention, 3399 Binsheng Road, Hangzhou 310051, E-Mail: [email protected]
Cite this as
Lyu X, Cai G, Liu K, Huang S, Yao J, et al. (2017) Analysis of Risk Factors for Development of Hepatocellular Carcinoma in Chronic HBV - Infected Liver Cirrhosis Patients: A Meta-Analysis. Int J Immunother Cancer Res 3(1): 034-040. DOI: 10.17352/2455-8591.000017The 5-year cumulative incidence rate of hepatocellular carcinoma (HCC) in chronic HBV -infected liver cirrhosis (LC) patients was up to 5%-30%. However, existing medical interventions can’t cure chronic HBV -infected LC patient. At present, the association between risk factors and development of chronic HBV -infected HCC have been explored by previous studies, but the results remains inconsistent. We took the chronic HBV -infected LC patients as the research object. We systematically searched for studies evaluating whether those proposed factors changed HCC risk from Chinese Medical Journal Database, Chinese National Knowledge Infrastructure, Pubmed, Elsevier, Springer, Wiley, OVID, EBSCO in BoKu data service platform. Odds ratios (OR) with 95% confidence intervals (CI) were calculated by Review Manager 5.0. In this meta-analysis, 1088 cases and 602 controls from 6 studies were included. Our results showed that pooled OR with 95% CI for the factors analyzed were: non-antiviral treatment 3.59(2.73, 4.72), high HBV DNA levels 3.12(2.29, 4.25), drinking alcohol 1.86(1.41, 2.26), a family history of HCC 10.12(4.23, 24.25), male gender 1.48(1.13, 1.95), smoking 2.93(1.99, 4.40), a history of diabetes mellitus 5.87(3.06, 11.27), a family history of HBV 1.20(0.92,1.57), a history of fatty liver 2.29(1.22,4.32) and HBeAg positive 2.05(1.15, 3.68), respectively. Non-antiviral treatment, high HBV DNA levels, drinking alcohol, smoking, a family history of HCC, male gender, a history of diabetes mellitus, a history of fatty liver and HBeAg positive can increase the development risk of HCC in chronic HBV -infected LC patients from currently available evidence.
Abbreviations
HCC: Hepatocellular Carcinoma; LC: Liver Cirrhosis; CI: Confidence Intervals; HBV: Hepatitis B Virus; Hbsag: Hepatitis B Virus Surface Antigen; Hbeag: Hepatitis B E Antigen; CNKI: National Knowledge Infrastructure; CMJD: Chinese Medical Journal Database; M: Model; F: Fixed-Effect Model; R: Rrandom-Effect Model.
Introduction
Liver cancer is the fifth most common carcinoma and the third most common cause of cancer-related deaths worldwide, resultting in about 500,000 deaths every year [1–3]. Liver cancer consists predominantly of HCC, in China, and the number of HCC accounts for 55% of all HCC cases in the world and the incidence of HCC is increasing now [4,5].
In view of a large of scale of the public health problem triggered by HCC, over the past few decades, some measures, reducing the lyngbya toxins in drinking water and reducing the aflatoxin content in food and inoculating Hepatitis B vaccine in all newborns to effectively block mother-to-infant HBV transmission, have been implemented in China [6–8]. However, the HBV infection rate of the adult still is high, and there are 9.3 million chronic HBV -infected people [9,10]. Moreover, the incidence of HCC still is increasing, in which HCC with chronic HBV -infected account for approximately 80% [11].
Whereas chronic HBV -infected LC patients will be the major source of HCC over the next 50 years, with LC rate of 70% -90% in HBV -infected HCC patients, and the 5-year cumulative incidence rate of HCC in chronic HBV -infected LC patients was up to 5% -30% [12]. However, existing medical interventions can’t cure chronic HBV -infected LC patients and the development of HCC goes through a long history.
At present, some behavior intervention measures have already prevented.
Chronic HBV -infected LC patient’s condition deterioration. Hence, our study focused on the chronic HBV -infected LC patients.
Previous studies have indicated the risk factors included a family history of HCC, smoking, high level of HBV replication and the use of alcohol, however the effects of these factors were controversial [13-19]. In view of a large of scale of the public health problem accompanied with chronic HBV -infected LC patients, the major risk factors for HCC development in chronic HBV -infected LC patients were analyzed to control the development of HCC.
Meta-analysis can implement statistical analysis for combining and contrasting results from different studies, and meta-analysis can reduce random error and identify associations or patterns in the context of a variety of evidence. In this study, we performed this meta-analysis to identify the associations between possible factors and the development of HCC with chronic HBV infection.
Materials and Methods
Literature and Search Strategy
All articles were retrieved from the following databases in BoKu data service platform: Chinese Medical Journal Database (CMJD), Chinese National Knowledge Infrastructure (CNKI), Pubmed, Elsevier, Springer, Wiley, OVID and EBSCO
Searches were performed via using the search field “Title/Abstract” and using the search terms (“cirrhosis” ) and (“hepatitis b”) and (“risk factor”) from PubMed, Elsevier, Springer, Wiley, OVID , EBSCO in BoKu data service platform. Searches were performed via using the search field “Abstract” and using the search terms (“cirrhosis” ) and (“hepatitis b”) and (“risk factor”) from CNKI and CMJD data journals published between January 2011 and September 2016.
The present study was carried out following Meta-analysis in PRISMA guidelines [20].
Inclusion and exclusion criteria
In our search, only primary studies were included. All eligible articles were case-control or cohort studies between January 2011 and September 2016 and the articles were published in Chinese or English.
Studies were included in the meta-analysis provided that: (1) the article was a cohort study or a case-control and the article had been publicated with full text available; (2) all cases and controls were diagnosed by national diagnostic criteria existing at that time, and possible risk factors were reported; and (3) the data was reported and can be used to calculate OR with 95% CI.
Studies were excluded from the meta-analysis when: (1) The article reported other forms of viral hepatitis (hepatitis A or C or D or E or G) as the etiological agent. (2) The article did not provide a workable value for the main variable.
Data extraction
Two independent reviewers finished an assessment using a standardized data extraction form designed by our group so as to decide whether an article should be included or excluded. Data were extracted from each study by two separate investigators.
Discrepancies between the decisions of the two reviewers were discussed. If a consensus was not achieved, a third reviewer made the last decision. Articles were examined to eliminate duplicate reports of the same research.
The following information was extracted from all of the acquired studies: the study type, the numbers of patients in each group, and the characteristics of each group at baseline (including female/male ratio, average and median ages). Definition of main outcomes: liver cirrhosis and HCC were diagnosed by the guidelines at that time [21,22].
Statistical analysis
The OR with 95% CI was used as the main outcomes to measure efficacy. Analyses were performed using Review Manager 5.0 (Cochrane Collaboration, Rigshospitalet, Denmark). The OR was not pooled when the number of OR of the risk factor were less than 4. All of the P-values were two-sided. Meta-analysis was performed using either the fixed-effect or random-effect model, depending on the statistical heterogeneity among studies as evaluated by Cochran’s chi-square test [23]. Statistical heterogeneity among studies was assessed using the Q and I2 statistics. In this meta-analysis, when p ≤ 0.1 the random-effect model was employed, and when p > 0.1 the fixed effects model was employed. In this meta-analysis, subgroup analyses were used to analyze the associations between different risk factors and HCC, and funnel plot were used to examine publication bias.
Results
Literature search
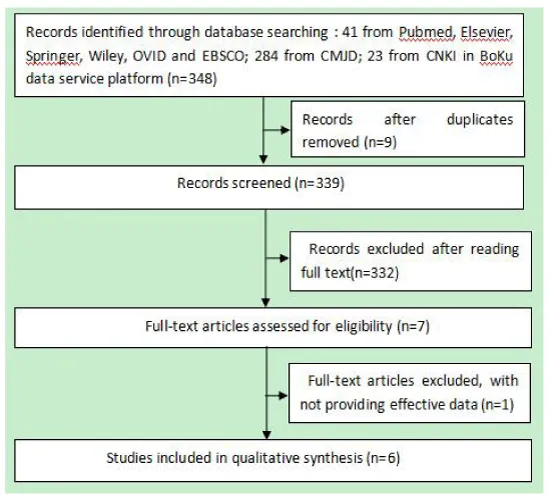
The selection of included studies in this meta-analysis was shown in figure 1.
According to the inclusive and exclusive criteria, all articles were retrieved and carefully reviewed to assess the eligibility. Six eligible studies were identified after screening of 348.
Characteristics of the studies
A total of 6 studies, including 1088 cases and 602 controls were included in our research. Among the six studies, following categories were studied: drinking alcohol (1690 cases), smoking (1690 cases), non-antiviral treatment (1450 cases), high HBV DNA levels (1543 cases), HBeAg positive (983cases), family histories of HCC (1356 cases), a history of diabetes mellitus (1690 cases), a family history of HBV (1225 cases), a history of fatty liver (1395 cases) and male gender (1690 cases). The details of all of the studies evaluated in this meta-analysis are shown in table 1 [14–19]. Six studies fulfilled the requirements and these included 1690 objects (Table 1).
The available sample size of each study was ranging from 120 to 715 objects. The mean age and the percentage of females also changed greatly (Table 1).
Effects of Related Factors on the Development of HCC
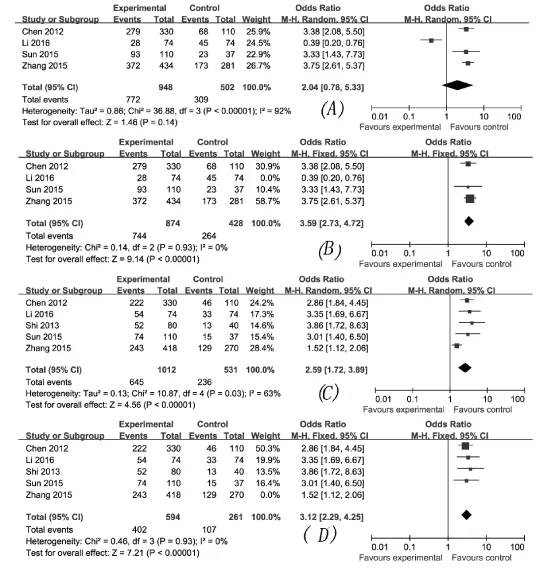
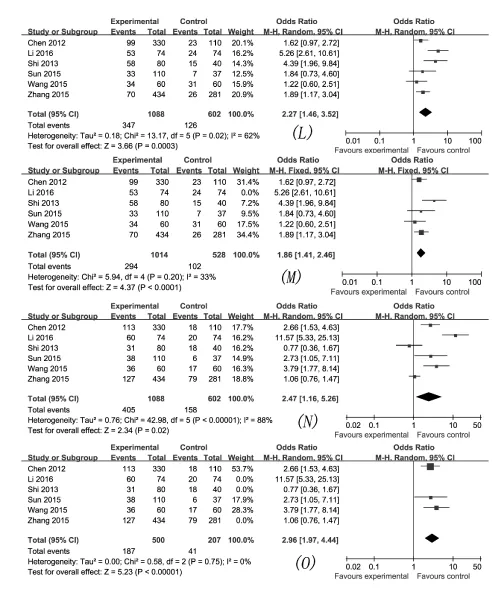
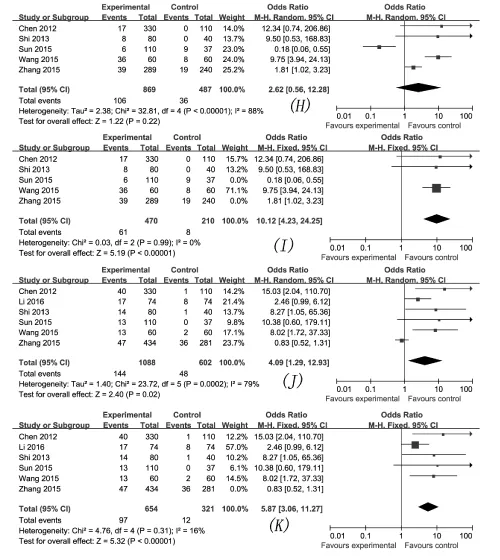
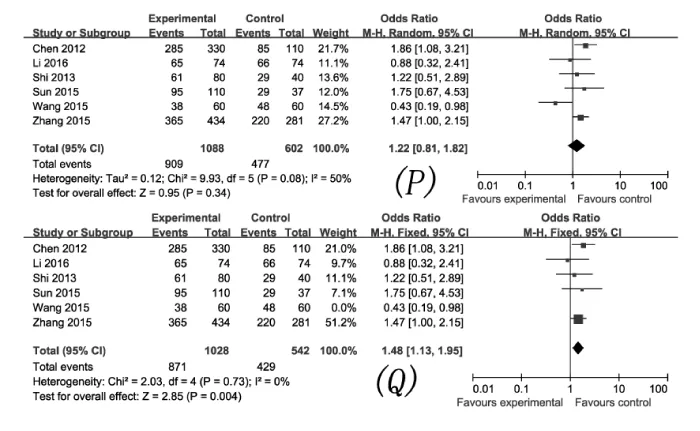
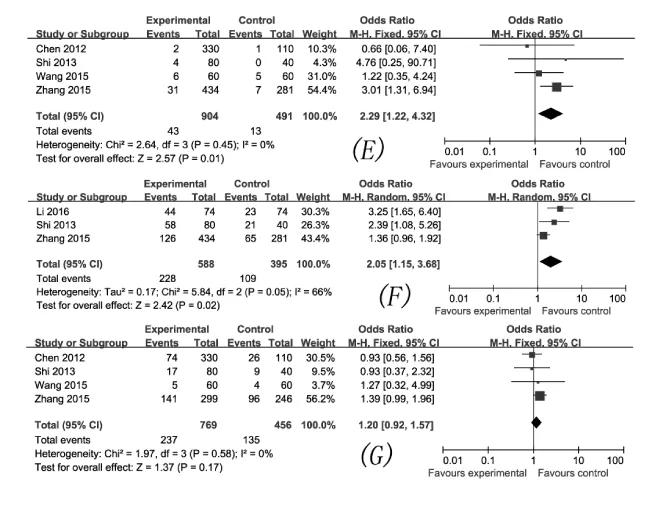
The effects of non-antiviral treatment (four studies, 1450 research objects), drinking alcohol (six studies, 1690 research objects), smoking (six studies, 1690 research objects), high HBV DNA levels (five studies, 1543 research objects), HBeAg positive (three studies, 983 research objects), family histories of HCC (five studies, 1356 research objects) a history of diabetes mellitus (six studies, 1690 research objects), a family history of HBV (four studies, 1225 research objects), a history of fatty liver (four studies, 1395 research objects) and gender (male) (six studies, 4984 research objects) on the development of HCC were investigated in this analysis and the results are displayed there (Figures 2–6), respectively.
The pooled OR with 95% CI for the ten factors investigated were: non-antiviral treatment 3.59 (2.73, 4.72), high HBV DNA levels 3.12 (2.29, 4.25), drinking alcohol 1.86 (1.41, 2.26), a family history of HCC 10.12 (4.23, 24.25), male 1.48 (1.13, 1.95), smoking 2.93 (1.99, 4.40), a history of diabetes mellitus 5.87 (3.06, 11.27), a family history of HBV 1.20 (0.92,1.57), a history of fatty liver 2.29 (1.22,4.32) and HBeAg positive 2.05 (1.15, 3.68), respectively.
The heterogeneity test showed that the variation of study-specific OR for high HBV DNA levels, non-antiviral treatment, drinking alcohol, smoking, a family history of HCC, a history of diabetes, HBeAg positive and male were statistically(p < 0.10), therefore, the results for these factors were pooled via using the random effect method. The heterogeneity test indicated that the variation of study-specific OR were not statistically significant (p > 0.10), therefore, the results for the other factors were pooled via using the fixed effect method. The results of statistical analysis and calculation are shown in table 2.
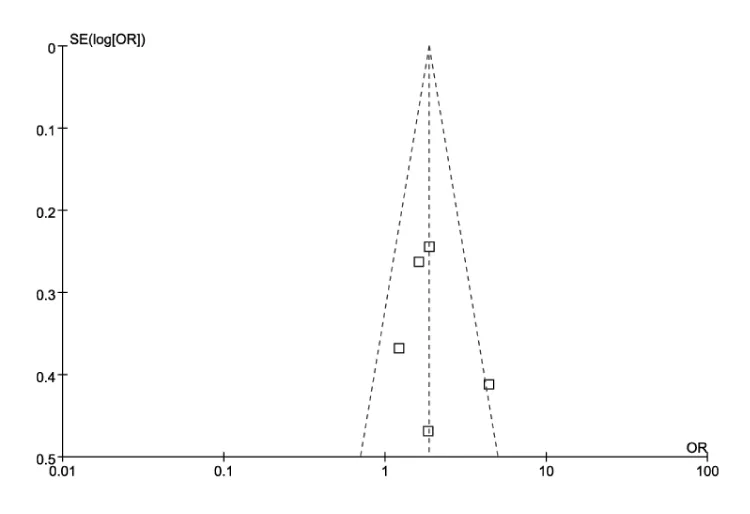
Sensitivity Analysis and Publication Bias
In some subgroups, in view of the enormous heterogeneity, we used sensitivity analysis to identify possible heterogeneous records from eligible studies. After omitting the selected studies, the study-specific OR results with lower degree of heterogeneity are shown in Table 3, and the effects of seven factors on the development of HCC are displayed in figure 3–6, respectively. A funnel plot for publication bias is displayed in figure 7.
Discussion
The development of HCC goes from liver damage to liver fibrosis to liver cell transformation, and multiple risk factors can affect progression of the development of HCC. In this study, we finished a comprehensive analysis of risk factors for the development of HCC with chronic HBV infection. In this meta-analysis, we collated literature to definite the association between possible factors and the development of HCC in chronic HBV -infected LC patients.
Our meta-analysis result indicated that, compared with not having the Corresponding factor, the chronic HBV -infected LC patients with high HBV DNA levels have more than threefold the risk of HCC development. Other studies also confirmed this findings [24,25]. This indicated that antiviral treatment could greatly decrease the number of HCC development in chronic HBV -infected LC patients.
Our meta-analysis result also indicated that, compared with not having the corresponding factor, drinking alcohol can increase the risk of HCC development. Drinking alcohol can result in chronic oxidative stress and cytokines production and can result in the development of HCC under chronic inflammation condition [26]. These findings also were confirmed by other studies [27,28]. In addition, this study showed that smoking can increase the risk of HCC development, and the results were confirmed by other study [29]. Furthermore, this study also showed that a history of liver fatty and a history of diabetes can increase the risk of HCC development, and the results were confirmed by other studies [30,31]. Since the proportion of the population with these risk factors is high in menfolk, professional health education should be enhanced to changes bad behavioral to control the development of HCC.
This study showed that a family history of HCC, non-antiviral treatment and male gender did not affect HCC development, After omitting those studies resulting in the development of heterogeneity, the above-mentioned three factors were associated with an increase risk in the development of HCC with chronic HBV infection [16,17,19]. A family history of HCC can increase the risk of HCC, and that may be connected with the genetic susceptibility to HCC and with the same carcinogenic factors exposed. In addition, this study also showed that a family history of hepatitis B did not affect HCC development, and the results were also different from that observed in previously reported research [27]. A possible reason for this was that the amount of information was not big enough. Confirmatory research should be done to confirm the real association between these factors and the risk of HCC development.
Heterogeneity in the variation of study-specific OR for high HBV DNA levels was determined. One possible reason was that unequal proportion of participants had received antiviral treatment in included study, and after omitting the study, the heterogeneity disappeared [17].
In addition, in the variation of study-specific OR for drinking alcohol and smoking, heterogeneity was found. One possible reason is that there was information bias in one retrospective study and three retrospective studies, respectively [15,17,19]. These studies were excluded, in the variation of study-specific OR for these two factors, and heterogeneity was not found.
In this study, in the variation of study-specific OR for a history of diabetes and a history of fatty liver, heterogeneity was found. One possible reason is that the patient’s age and patient’s illness vary slightly from study to study anyhow [15-17,19]. These studies were excluded, in the variation of study-specific OR for these two factors, and heterogeneity was not found.
This study has several limitations: (1) In our analysis, six eligible studies were included, and the sample size was limited in subgroup analysis which could have small affected the results. (2) Some non-randomized designs and retrospective studies are susceptible to various biases, for example, selecting inappropriate subjects. These biases could have decreased slightly the internal and external validity of this study. (3)Publication bias could exist in some subgroup analyses, in view of the low possible publication rate for negative studies.
Conclusions
This meta-analysis draw a conclusion that non-antiviral treatment, high HBV DNA levels, drinking alcohol, smoking, a family history of HCC, male gender, a history of diabetes mellitus, a history of fatty liver and HBeAg positive can increase the development risk of HCC in chronic HBV - infected LC patients from currently available evidence.
Authors’ contributions
Jianmin Jiang, Xiang Lyu, Zhifang Wang, Huakun Lv, and Yongdi Chen designed the study. Xiang Lyu and Kui Liu did the statistical analysis. Xiang Lyu, Sichao Huang, Zhengting Wang, Gaofeng Cai, Jun Yao, Zhenggang Jiang and Zhengting Wang prepared the manuscript. Jianmin Jiang, Huakun Lv, and Yongdi Chen did the critical review of the manuscript. All authors read and approved the final manuscript.
This work was supported by Ministry of Science and Technology supporting the National Scientific and Technological Major Project of China (grant numbers No. 2013ZX10004–904, 2013) and National Natural Science Foundation of China (grant numbers No. 31500751, 2015).
- Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics 2002. CA Cancer J Clin 55: 74-108. Link: https://goo.gl/3wCtmd
- Gomaa AI, Khan SA, Toledano MB, Waked I, Taylor-Robinson SD (2008) Hepatocellular carcinoma: Epidemiology risk factors and pathogenesis. World J Gastroenterol 14: 4300-4308. Link: https://goo.gl/zewv8w
- Bosch FX, Ribes J, Cléries R, Díaz M (2005) Epidemiology of hepatocellular carcinoma. Clin Liver Dis 9: 191-211. Link: https://goo.gl/eJm1ZK
- Stewart BW, Wild C (2014) World Cancer Report 2014, World Health Organization: Lyon France 2014. Link: https://goo.gl/UEHA7C
- Zhang S, Zheng R, Li N, Zeng H, Dai Z, et al. (2012) Analysis and prediction of liver cancer incidence in China 46: 587-592. Link: https://goo.gl/WvJsKr
- Zhang YZ, Li X, Zhou WJ, Niu WM, Liu P, et al. (2012) Study on microcystins-LR pollution situation of Taihu rim. J Food Saf Q 3: 700-704. Link: https://goo.gl/zjtDHz
- Zhang WH (1995) The role of Chinese herbal medicine in the elimination of aflatoxin. Food Storage 4 :82-85.
- Shandong Lu Hua (2008) Group Co Ltd Squeezing methods of oil production and technology of getting rid of aflatoxin. Food Saf Guide 1: 81-83.
- Liang X, Bi S, Yang W, Wang L, Cui G, et al. (2013) Epidemiological serosurvey of Hepatitis B in China-Declining HBV prevalence due to Hepatitis B vaccination. Vaccine 31: 21-28. Link: https://goo.gl/XCV7oB
- Liang X, Bi S, Yang W, Wang L, Cui G, et al. (2009) Evaluation of the impact of hepatitis B vaccination among children born during 1992-2005 in China. J Infect Dis 200: 39-47. Link: https://goo.gl/PyLRqQ
- Huang GY, Ma XG, Wang CC (2005) Heavy drinking alcohol can enhance risk of hepatocellular carcinoma associated with hepatitis B virus infection. J Oncol 12: 405-408. Link: https://goo.gl/srqYxU
- El-Serag HB (2012) Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 142: 1264-1273. Link: https://goo.gl/Eo3fqD
- Lyu X, Liu K, Chen Y, Wang Z, Yao J, et al. (2016) Analysis of Risk Factors Associated with the Development of Hepatocellular Carcinoma in Chronic HBV-Infected Chinese: A Meta-Analysis. Int J Environ Res Public Health 13: 6-30. Link: https://goo.gl/o8czwB
- Chen P, Li J, Su F, Li JB, Cheng F (2012) Risk factors for hepatocellular carcinomas in patients with liver cirrhosis. Acta Univ Anhui 47: 1218-1221.
- Shi CZ, Xue F, Sun YF (2013) Evaluation of Risk Factors of Primary Hepatic Carcinoma Due to Hepatitis B Cirrhosis. Pract J Cancer 28: 399-401. Link: https://goo.gl/bnhEuE
- Wang XL (2015) Analysis of related risk factors of hepatitis B-induced liver cirrhosis complicated with primary hepatic carcinoma. China Practical Medical 16: 38-40.
- Zhang YQ, Peng LJ, Cao YR, Zeng ZP, Wu YJ, et al. (2015) Analysis of risk factors for hepatocellular carcinomas in patients with Chronic HBV-Infected liver cirrhosis. Chinese Journal of Hepatology 23: 512-516. Link: https://goo.gl/kg7mUB
- Sun GZ (2015) Analysis of risk for hepatocellular carcinomas in patients with hepatitis B. The Journal of Medical Theory and Practice 28: 203-204. Link: https://goo.gl/ivFLoq
- Li L, Yang WW, Wei T, Liu ZY, He TL (2016) Logistic analysis of risk for hepatocellular carcinomas in patients with chronic HBV-Infected liver cirrhosis. Chinese Journal of Gerontology 36:1653-1654. Link: https://goo.gl/npRxe9
- (2016) Key Documents.Accessed 8 October. Link: https://goo.gl/X3gFSR
- (2016) Chinese Anti-Cancer Association and the Professional Committee of Liver Cancer Clinical Oncology Collaboration Committee, China HCC Medical Association Hepatology Study Group. Diagnosis and treatment of primary liver cancer experts from standardization knowledge. J Clin Oncol 14: 259-269. Link: https://goo.gl/zKZUmD
- Zhonghua Liu Xing Bing Xue Za Zhi (2011) Chinese Society of Hepatology and Chinese Society of Infectious Diseases Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B 32: 405-415. Link: https://goo.gl/kF1MN6
- Dersimonian R, Laird N (1986) Meta-analysis in clinical trials. Controll Clin Trials 7: 177-188. Link: https://goo.gl/bo5tKe
- Thiele M, Gluud LL, Dahl EK, Krag A (2012) Antiviral therapy for prevention of hepatocellular carcinoma and mortality in chronic hepatitis B: systematic review and meta-analysis. BMJ Open. Link: https://goo.gl/wba2HY
- Liu J, Yang HI, Lee MH, Lu SN, Jen CL, et al. (2014) Spontaneous seroclearance of hepatitis B seromarkers and subsequent risk of hepatocellular carcinoma. Gut 63: 1648-1657. Link: https://goo.gl/5CThvE
- Mercer KE, Hennings L, Ronis MJ (2015) drinking alcohol Wnt/?-catenin signaling and hepatocarcinogenesis. Adv Exp Med Biol 815:185-195. Link: https://goo.gl/zehce5
- Li Y, Zhang Z, Shi J, Jin L, Wang L, et al. (2015) Risk factors for naturally-occurring early-onset hepatocellular carcinoma in patients with HBV-associated liver cirrhosis in China. Int J Clin Exp Med 8 : 1205-1212. Link: https://goo.gl/DKF32a
- Kim SS, Hwang JC, Lim SG, Ahn SJ , Cheong JY, et al. (2014) Effect of virological response to entecavir on the development of hepatocellular carcinoma in hepatitis B viral cirrhotic patients: comparison between compensated and decompensated cirrhosis. Am J Gastroenterol 109: 1223-1233. Link: https://goo.gl/o66v3i
- Jiang Y, Qin CY (2010) The Association of Cigarette Smoking with PDCD4 in Hepatocellular Carcinoma [D]. Shandong University. Link
- Wang P, Kang D, Cao W, Wang Y, Liu Z (2012) Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev 28: 109-122. Link: https://goo.gl/oeqRts
- White DL, Kanwal F, El-Serag HB (2012) Association Between Nonalcoholic Fatty Liver Disease and Risk for Hepatocellular Cancer Based on Systematic Review. Clin Gastroenterol Hepatol 10: 1342-1359. Link: https://goo.gl/PVzuxv
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
