International Journal of Immunotherapy and Cancer Research
Osteotropism of Breast and Prostate Cancer: Clinical and Experimental Perspective
Manuel Scimeca1-3#, Francesca Starace1#, Deborah Gratti1, Viviana Benedicta Sapia1, Rita Bonfiglio1 and Elena Bonanno1*
2OrchideaLab S.r.l., via del Grecale 6, Morlupo, Rome (RM), Italy, www.orchidealab.it
3IRCCS San Raffaele Pisana, 00166, Rome, Italy
#Manuel Scimeca and Francesca Starace equally contributed to the work
Cite this as
Scimeca M, Starace F, Gratti D, Sapia VB, Bonfiglio R, et al. (2017) Osteotropism of Breast and Prostate Cancer: Clinical and Experimental Perspective. Int J Immunother Cancer Res 3(1): 032-033. DOI: 10.17352/2455-8591.000016Short Communication
Breast and prostate cancer are the two most common invasive cancers in women and men, respectively. Although these cancers arise in organs that are different in terms of structure and function, both organs require sexual hormones for their development, and tumors that arise from them are typically hormone-dependent and have extraordinary affinity each other [1]. That breast and prostate cancer share several biological, genetic and epidemiological aspects is known since 1950s. Pioneering studies designed to ascertain the genetic bases of breast cancer detected a higher frequency of prostate cancer among the relatives of women with breast cancer, which led them to propose that prostate cancer could be the male equivalent of at least some female mammary carcinomas [2].
One of the most important similitudes between breast and prostate tissues is represented by the fact that their malignant counterpart frequently show osteotropism. The presence of calcium deposits may represent the biological evidence that both breast and prostate cancers share with bone tissues. Moreover, several clinical and biological data prove that morphological appearance and elemental composition of calcifications could be related to patient’s prognosis [3]. It is known that microcalcifications are localized deposits of calcium, and they have been characterized according to their molecular composition as: TYPE I - composed of calcium oxalate (CO), TYPE II - composed of hydroxyapatite (HA) and TYPE III – composed of hydroxyapatite magnesium substituted Mg-Hap [4]. Recent studies have also investigated the molecular mechanisms involved in the formation of HA microcalcification in breast cancer demonstrating that this mineralization phenomenon could be comparable to that observed in physiological bone formation [5,6]. Specifically, in our recent study, we characterized the cells involved in the formation of breast microcalcification calling them Breast Osteoblast like-cells (BOLCs) [3,4]. The presence of BOLCs in ducts is due to development of epithelial to mesenchymal transition (EMT) as a result of specific stimuli, Transforming Growth Factor-β (TGFß) and Bone Morphogenetic Proteins (BMPs), that induced mammary cells to gain mesenchymal characteristics, transforming themselves into cells with an osteoblast-like phenotype [4,7].
For a long time BMPs have been considered only in relation to bone, but recently more thorough studies have been conducted to better understand their role in other organs and other pathways (including pathological such as cancer onset). These cytokines, belonging to the TGF- β super-family, play multiple physiological functions, but it has also been demonstrated, through this years, their involvement in promotion of oncogenic behavior by affecting apoptosis, invasion and angiogenesis, EMT phenomenon [8,9].
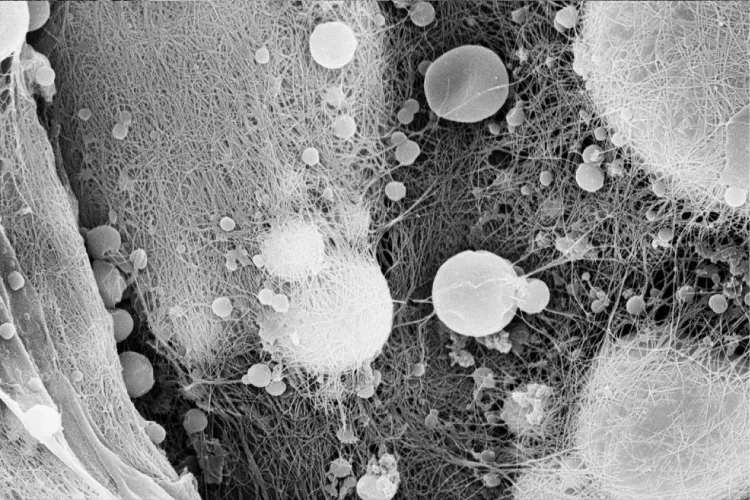
The most important clinical evidence of osteotropism is represented by the high frequency in which breast and prostate cancer metastasize into bone [10]. The type of bone metastases formed in breast cancer is a reflection of the local interaction between tumor cells and the bone remodeling system - a complex mechanism which remains to be fully characterized [10]. Bone metastases in breast cancer are most often osteolytic (characterized by destruction of normal bone), but can also be osteoblastic (involving the deposition of newly formed bone), or mixed [10]. The development of either osteolytic or osteoblastic lesions results from functional interactions between tumor cells and osteoclasts or osteoblasts, respectively (Figure 1). In contrast to breast cancer, prostate metastasis to the bone often results in osteoblastic lesions [10]. Still, it is known that prostate cancer lesions display both blastic and lytic characteristics during the early phases of the metastatic process [11]. There is evidence that, in prostate cancer, osteoblastic metastases form at sites of osteolytic lesions, suggesting an overall increase of bone remodeling at these sites [11]. Although the mechanisms of osteoblastic and osteolytic responses in prostate cancer are not fully understood, it is clear that many factors involved in osteolytic breast cancer bone metastasis also regulate the osteolytic aspects of prostate cancer. Noteworthy, our preliminary data showed a strictly association between the presence of osteoblast-like cells in primary mammary lesions and the occurrence of osteolytic bone metastasis (data not shown). It is important to note that both in breast and prostate cancer the main molecules involved in acquiring of osteotropism seem to be RANKL, RUNX2 and vitamin D receptor [10].
The finding of breast and prostate cancer cells with high affinity for bone environment could open new perspectives on prevention and therapy of bone metastases. Indeed, the characterization of the specific morphological-molecular profile of these cells can represent an extraordinary opportunity to identify markers for both early diagnosis and development of new drugs. Specifically, the use of molecules involved in the modulation of bone metabolism, such as anti-RANKL antibodies, could represent an extraordinary opportunity for the prevention of the development of bone metastasis from breast and prostate cancers. Similarly, pre-emptive administration of bone resorption inhibitors (e.g. bisphosphonates) or molecules with anti-osteoblastic effects (e.g. non-steroidal anti-inflammatory drugs) could possibly avoid the onset of the metastatic process. Nevertheless, further studies are needed to elucidate the exact molecular mechanism by which osteoblast-like cells form bone metastases.
The authors wish to thanks Orchidea Lab S.r.l. for technical support.
Disclosure
The study is original and the manuscript has not been published yet and is not being considered for publication elsewhere in any language either integrally or partially except as an abstract. All authors have agreed with the submission in its present (and subsequent) forms.
- Risbridger GP, Davis ID, Birrell SN, Tilley WD (2010) Breast and prostate cancer: more similar than different. Nat Rev Cancer 10: 205-212. Link: https://goo.gl/uwKg0g
- López-Abente G, Mispireta S, Pollán M (2014) Breast and prostate cancer: an analysis of common epidemiological features in mortality trends in Spain. BMC Cancer. Link: https://goo.gl/8WaUYj
- Scimeca M, Antonacci C, Bonanno E (2015) Breast Microcalcifications: A Focus. J Cell Sci Ther.
- Scimeca M, Giannini E, Antonacci C, Pistolese CA, Spagnoli LG, et al. (2014) Microcalcifications in breast cancer: an active phenomenon mediated by epithelial cells with mesenchymal characteristics. BMC Cancer 23: 14:286. Link: https://goo.gl/D4l1zO
- Cox RF, Morgan MP (2013) Microcalcifications in breast cancer: Lessons from physiological mineralization. Bone 53: 437-450. Link: https://goo.gl/YYXube
- Cox RF, Jenkinson A, Pohl K, O'Brien FJ, Morgan MP (2012) Osteomimicry of mammary adenocarcinoma cells in vitro; increased expression of bone matrix proteins and proliferation within a 3D collagen environment. Link: https://goo.gl/zBQ7WQ
- Scimeca M, Antonacci C, Colombo D, Bonfiglio R, Buonomo OC, et al. (2016) Emerging prognostic markers related to mesenchymal characteristics of poorly differentiated breast cancers. Tumour Biol 37: 5427-5435. Link: https://goo.gl/SG5Oap
- Alarmo EL, Kallioniemi A (2010) Bone morphogenetic proteins in breast cancer: dual role in tumourigenesis? Endocr Relat Cancer 17: 123-139. Link: https://goo.gl/PSNKjL
- Gonzalez DM, Medici D (2014) Signaling mechanism of the epithelial-mesenchymal transition. Sci Signal. Link: https://goo.gl/Ztkk3h
- Weidle UH, Birzele F, Kollmorgen G, Rüger R (2016) Molecular Mechanisms of Bone Metastasis. Cancer Genomics Proteomics 13: 1-12. Link: https://goo.gl/tJdo7M
- Ziaee S, Chu GC, Huang JM, Sieh S, Chung LW (2015) Prostate cancer metastasis: roles of recruitment and reprogramming, cell signal network and three-dimensional growth characteristics. Transl Androl Urol 4: 438-454. Link: https://goo.gl/k2LA5j
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
